The Centers for Medicare & Medicaid Services (CMS) is once again at the forefront of healthcare innovation with the introduction of the CMS TEAM Model. This groundbreaking initiative, part of the fiscal year 2025 Hospital Inpatient Prospective Payment Systems (IPPS) rule, aims to drive value-based care through a mandatory, episode-based payment model. Here’s a closer look at what the CMS TEAM model FY 2026 entails and what it means for the future of healthcare.
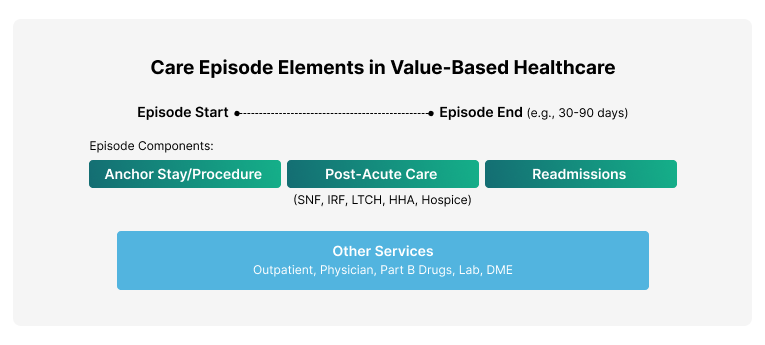
Key Elements of a Care Episode in Value-Based Healthcare
- Total cost of care for the entire episode
- Almost all expenditures included, with some exclusions
- Services can be received from any provider
- All sites of care are included
What is CMS TEAM Model?
The CMS TEAM model is designed to enhance the quality and cost-effectiveness of care provided to Medicare beneficiaries. Scheduled to commence on January 1, 2026, and run through December 31, 2030, this model focuses on holding hospitals accountable for the cost and quality of care during specific episodes of care. Here are the key components of the model:
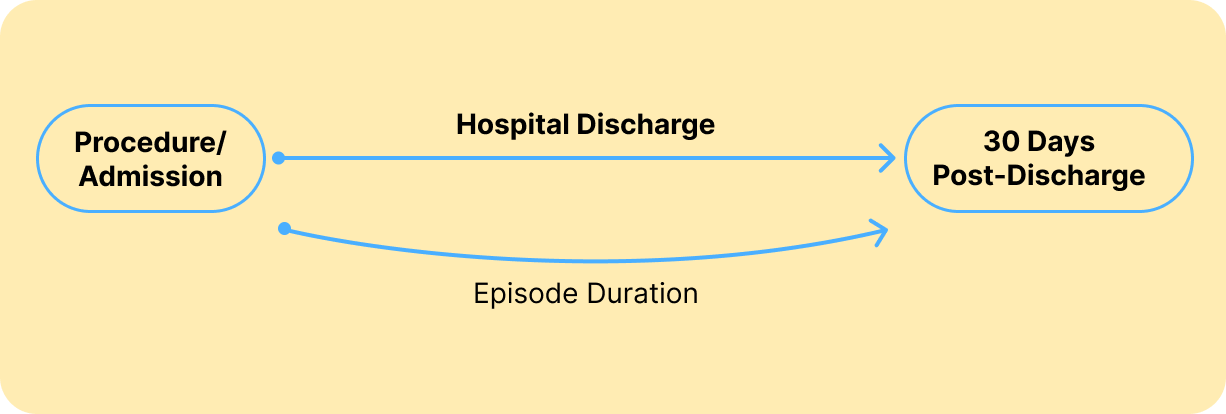
Episode Initiation and Duration
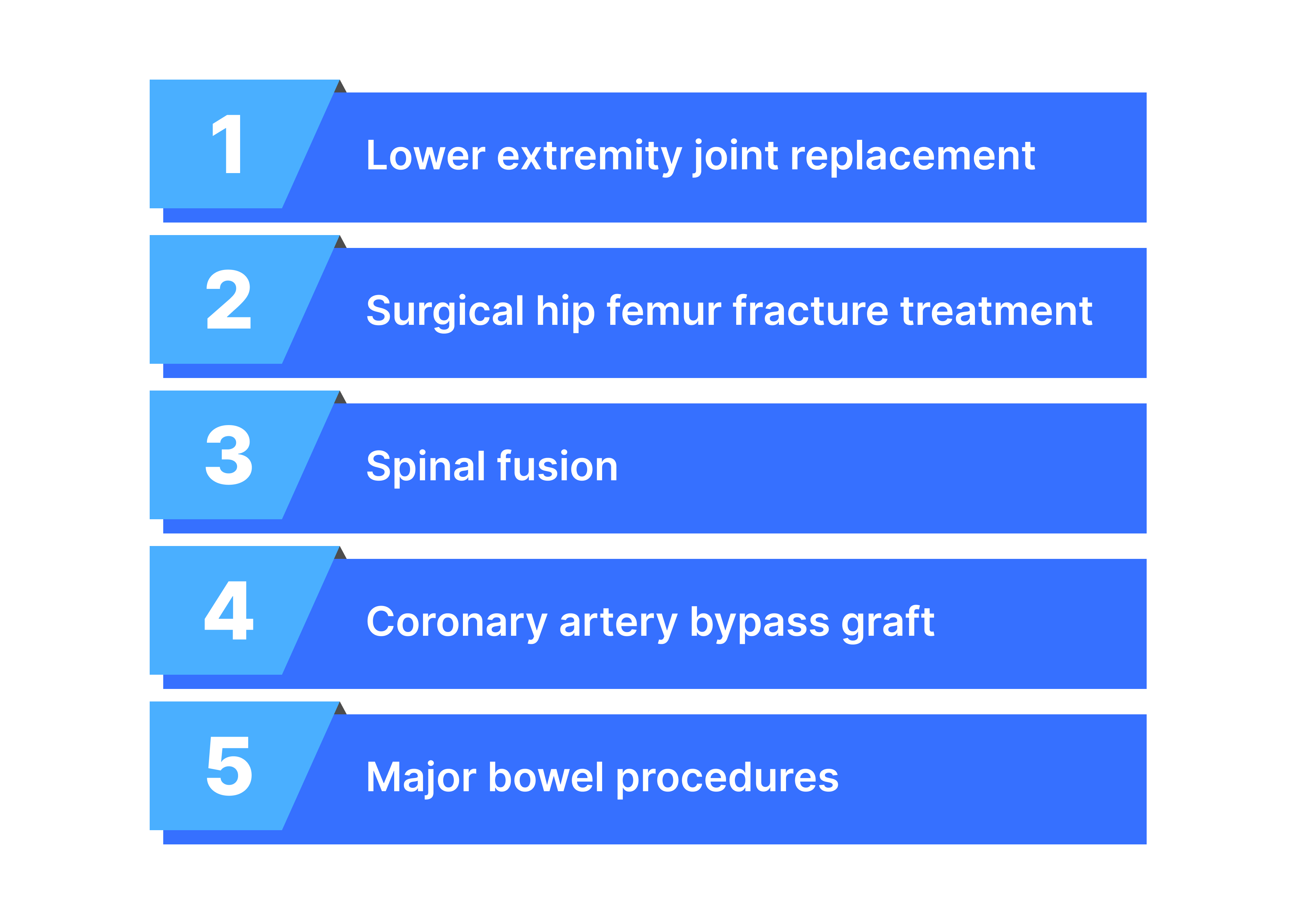
- Procedures Covered: The model covers the following procedures:
2. Episode Length: Each episode begins with the surgical procedure or hospital admission and continues for 30 days post-discharge. This timeframe aims to keep the model focused on costs and care quality that hospitals can directly influence.
HCPCS-to-MS-DRG Mapping for Comprehensive Coverage
A critical technical component of TEAM is how it handles episodes initiated in different care settings. CMS will map outpatient HCPCS procedure codes to corresponding MS-DRGs for episodes initiated in outpatient settings. This sophisticated mapping process ensures consistency in applying bundled-payment logic across both inpatient and outpatient care, creating a seamless payment model regardless of where the triggering procedure occurs. This approach eliminates potential gaps or inconsistencies that could arise from treating inpatient and outpatient episodes differently.
TEAM Participants
- Eligible Participants: The model is limited to acute care hospitals paid under the IPPS.
2. Selection Methodology: Hospitals in selected Core Based Statistical Areas (CBSAs) must participate, with CMS using stratified random sampling to choose roughly a quarter of eligible CBSAs.

To incentivize cost control, CMS sets price targets for each episode. Hospitals that spend below these targets can receive additional payments, while those exceeding the targets may face recoupments. Payments and recoupments are adjusted based on the hospital’s performance on quality measures, ensuring that both cost and care quality are prioritized.
Regional & Hospital-Level Target Price Calculation
The TEAM model employs a sophisticated dual-level approach to target price calculation that ensures both regional consistency and hospital-specific fairness.
Regional-Level Pricing Foundation
CMS computes target prices at the regional level (by MS-DRG/HCPCS and U.S. Census Division) using three years of historical regional spending data. This data is then trended forward and normalized to account for inflation and healthcare cost trends, creating a robust baseline for each episode type within specific geographic regions.
Hospital-Specific Adjustments
Building upon the regional foundation, CMS also calculates hospital-level target prices with specific adjustments to ensure fairness across different hospital types and patient populations. This dual approach means that while hospitals compete within consistent regional benchmarks, they’re also evaluated fairly based on their unique circumstances and patient mix.
The target price calculation process follows these steps:
1. Start with a benchmark price for the specific DRG/HCPCS episode type in the census region, based on the three-year baseline
2. Apply site-neutral targets for certain HCPCS/DRG combinations within LEJR and Spinal Fusion episode groups
3. Apply comprehensive multi-level risk adjustments (detailed below)
4. Implement quality-adjusted pricing with specific discount factors
Quality-Adjusted Pricing with Strategic Discount Factors
Target prices incorporate quality-adjusted pricing mechanisms with episode-specific discount factors designed to drive efficiency while maintaining quality. The model applies:
· 1.5% discount for Coronary Artery Bypass Graft (CABG) and Major Bowel Procedure episodes
· 2.0% discount for LEJR, Surgical Hip/Femur Fracture Treatment (SHFFT), and Spinal Fusion episodes
Importantly, final reconciliation amounts are adjusted by hospitals’ Composite Quality Scores, creating a direct link between quality performance and financial outcomes.
Comprehensive Multi-Level Risk Adjustment
TEAM incorporates one of the most sophisticated risk adjustment methodologies among Medicare payment models, operating at both patient and hospital levels to ensure equitable target price calculations.
Patient-Level Risk Adjustment
The patient-level risk adjustment includes:
· Age brackets for demographic considerations
· Multiple HCC (Hierarchical Condition Category) variables – up to 16 HCC variables depending on episode type – providing granular adjustment for patient complexity
· Social risk factors to account for social determinants of health that impact care costs and outcomes
Hospital-Level Risk Adjustment
Hospital-level adjustments account for institutional characteristics:
· Hospital bed size adjustments recognizing operational differences between facility sizes
· Safety net hospital status to protect hospitals serving vulnerable populations
This comprehensive dual-level approach ensures that target prices reflect both the complexity of individual patients and the operational realities of different hospital types, promoting fairness while maintaining accountability.
CMS TEAM Model Quality Measures & Composite Quality Score (CQS)
CMS TEAM Model incorporates quality measures linked to financial gains and losses, ensuring that participants focus on both cost reduction and quality improvement. The key quality measures include:
1. Hybrid All-Cause Readmission Measure
2. CMS Patient Safety Indicator 90 (PSI-90)
3. Lower Extremity Joint Replacement (LEJR) Patient-Reported Outcome-Based Performance Measure
4. Hospital Harm and Failure to Rescue Measures (beginning in Performance Year 2)
CMS will use these measures to calculate a Composite Quality Score (CQS), similar to those used in BPCI-Advanced and other Medicare alternative payment models. This score directly impacts the financial reconciliation process.
The Composite Quality Score (CQS) combines these measures, weighted by episode volume, to determine a hospital’s quality performance. The CQS then adjusts the financial reconciliation amounts, rewarding hospitals that achieve high quality scores and reducing the financial burden on those that do not.
The TEAM model, like BPCI Advanced and CJR, focuses on specific types of care episodes. These episodes are triggered by certain surgical procedures, which can occur either during an inpatient hospital stay or an outpatient visit. The procedures are identified using standardized coding systems: Medicare Severity Diagnosis-Related Groups (MS-DRGs) for inpatient procedures, and Healthcare Common Procedure Coding System (HCPCS) codes for outpatient procedures.
Health Equity Requirements in CMS TEAM Model
The Transforming Episode Accountability Model (TEAM) emphasizes improving health equity and access to high-quality care for people in underserved areas. To support this goal, TEAM incorporates several health equity-focused elements. Participants are required to screen each beneficiary for at least four health-related social needs (HRSNs), including food insecurity, housing instability, transportation needs, and utilities difficulties. Additionally, participants may voluntarily submit health equity plans that identify health disparities, set health equity goals, and outline strategies for improving health equity.
The model also encourages demographic data reporting, which may include information on race, ethnicity, language, disability, sexual orientation, gender identity, and other characteristics. By integrating these components, TEAM aims to address disparities in healthcare delivery and outcomes, ensuring that value-based care initiatives benefit all patient populations equitably.
List of Eligible Hospitals
The Center for Medicare and Medicaid Innovation (CMMI) has recently released a list of hospitals for CMS TEAM.
Primary Care and Specialty Care Coordination
The CMS TEAM model emphasizes the importance of coordination between primary care and specialty care providers to improve patient outcomes and reduce costs. Key aspects of this coordination include:
- Primary Care Referral: TEAM participants are required to provide a referral to a primary care provider prior to discharge from the hospital or outpatient surgical facility for all beneficiaries. This ensures continuity of care and helps manage post-acute care needs.
- Follow-up Care: The model tracks patient follow-up rates, including both primary care and specialist visits. For example, the document mentions monitoring the percentage of patients who have either a Transitional Care Management (TCM) or Primary Care Provider (PCP) visit within 14 days of the episode, as well as specialist follow-up within 30 days.
- Care Continuum Management: TEAM encourages participants to implement strategies for coordinating care across the entire episode, including post-acute care settings such as skilled nursing facilities, home health agencies, and rehabilitation facilities.
- Financial Impact: The model creates financial incentives for specialists to move towards value-based care and for primary care providers to engage with specialists. This alignment of incentives aims to foster better collaboration between primary and specialty care.
- Existing Value-Based Care Initiatives: Organizations participating in other value-based care models (such as the Medicare Shared Savings Program) may benefit from integrating TEAM operations with these initiatives, potentially sharing resources and governance structures to enhance care coordination.
Watch our Podcast and lean how hospitals and ACOs can prepare for CMS TEAM Implementation.
Future Directions – CMS TEAM Model
CMS aims to use the TEAM model to build on the lessons learned from previous episode-based models like the Comprehensive Care for Joint Replacement (CJR) and Bundled Payments for Care Improvement Advanced (BPCI Advanced). If successful, TEAM could set a new standard for managing episodes of care within Traditional Medicare.
To protect safety net hospitals, CMS is exploring adjustments to regional target prices, ensuring these hospitals are not disproportionately penalized. The agency is actively seeking feedback on these adjustments to refine the model before its implementation.
How hospitals should prepare for CMS TEAM model (2026–2030)
As TEAM launches on January 1, 2026, hospitals must act swiftly to prepare. Beginning in Fall 2024, organizations should conduct a thorough assessment of their current performance in TEAM episodes and identify areas for improvement. Throughout 2025, focus should shift to developing strategies for enhancing performance and ensuring compliance with model requirements. Key preparation areas include discharge planning, care coordination, outcomes management, and implementing mandatory elements like beneficiary notification and HRSN screening.
Organizations should also establish data analysis systems to track performance indicators. Early preparation is crucial due to TEAM’s mandatory nature for selected hospitals, the late provision of CMS data, and the model’s significant financial implications. By taking proactive steps, hospitals can position themselves for success in TEAM, potentially improving both clinical outcomes and financial performance in this value-based care model.
Conclusion
The Transforming Episode Accountability Model (TEAM) represents a significant step forward in CMS’s efforts to promote value-based care. By aligning financial incentives with quality performance, TEAM aims to improve patient outcomes while controlling healthcare costs. Hospitals and healthcare providers should prepare for this new model, which promises to reshape the landscape of Medicare payment and care delivery in the coming years.
Book a Demo Now to see how Persivia can help you optimize episode performance, improve quality scores, and achieve sustainable financial success under TEAM.
Table of Contents