This blog compares the top 5 care management software platforms in 2025: Persivia CareSpace®, AthenaOne®, Cerner HealtheIntent®, Epic Care Everywhere® & HealthEdge GuidingCare®. It breaks down their real-world impact, key features, and best use cases. Ideal for healthcare leaders choosing tools for better care coordination, reduced readmissions, and improved patient engagement.
Every preventable hospital readmission drains millions from healthcare budgets and pushes clinicians to the brink of burnout. Fragmented care coordination leaves patients lost in the system, hopping between providers with no clear path forward. Without a unified, smart solution, these costly breakdowns will only worsen.
Care management software solves these coordination breakdowns by connecting providers, automating workflows, and using predictive analytics to identify patients who need attention before emergencies develop. The right platform delivers substantial administrative cost reductions while improving readmission rates. The wrong choice drains budgets while making everything more complicated.
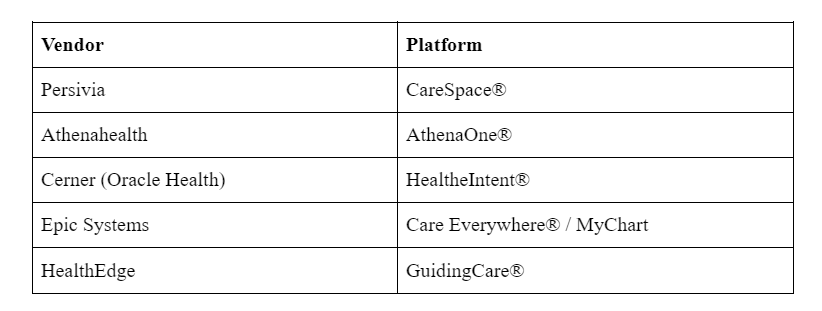
Here are the 5 Care Management Software Vendors that have built platforms that deliver measurable results instead of creating new problems.
Choosing the right care management software determines whether your organization thrives or struggles for the next decade. Here’s what separates the leaders from the laggards, backed by real performance data and implementation insights.
What Is Care Management Software?
Care management software coordinates patient care across multiple providers, locations, and periods to eliminate the fragmented care that leads to readmissions and poor outcomes. These platforms track health data, manage treatment plans, and ensure care teams communicate effectively about patient status and next steps.
The software integrates with existing electronic health record systems to build comprehensive patient profiles that follow individuals throughout their healthcare journey. Care teams can monitor chronic conditions, schedule proactive interventions, and identify high-risk patients before problems escalate into expensive emergency department visits.
Essential capabilities that drive results
- Patient risk stratification using predictive analytics
- Automated care plan creation and real-time updates
- Multi-provider communication and care coordination
- Automated quality reporting and regulatory compliance
- Revenue cycle optimization with cost tracking
- Patient engagement portals and self-service tools
Top 5 Care Management Software Vendors in 2025
1. Persivia CareSpace® – AI-Powered Predictive Care Management
Persivia CareSpace® is an end-to-end AI-powered care management platform that supports the complete care management lifecycle, from risk stratification, provider and patient engagement, prior authorization, through to actionable insights at the point of care (POC) and care management analytics. The platform achieves this by integrating multiple advanced AI technologies into a single platform.
The following are the key components of this solution:
• Data Integration: Aggregates and harmonizes clinical, claims, social determinants of health (SDOH), device, behavioral, and patient-reported data into a unified longitudinal patient record, breaking down data silos for a comprehensive view.
• AI-Driven Insights & Analytics: Employs Persivia’s Soliton® – AI Engine to deliver predictive, prescriptive, and generative AI insights that identify risks, care gaps, and opportunities, enabling data-driven clinical and operational decisions in real time.
• Personalized Care Plans: Generates automated, patient-specific care plans using a library of over 200 clinical programs and evidence-based pathways tailored to individual risk profiles and clinical needs.
• Point of Care Integration: Integrates bi-directionally with major EHRs via CareTrak®, delivering actionable alerts.
• Risk Stratification: Continuously stratifies patient populations by analyzing longitudinal data to identify high-risk individuals and prioritize interventions effectively.
• Care Gaps Identification: Detects and highlights clinical care gaps and preventive opportunities, supporting proactive management and quality improvement initiatives.
• Patient Outreach: Uses generative AI to automate personalized, multi-channel patient communications, improving engagement, adherence, and care coordination.
• Workflow Integration: Automates complex care management workflows, including assessments, care planning, and quality measure reporting, reducing clinician burden and enhancing operational efficiency.
• Advanced Cost and Utilization Analytics: Provides detailed analytics on healthcare utilization and costs across care settings, enabling organizations to optimize resource use and reduce unnecessary services.
• Resource Prioritization: Aligns care management resources by prioritizing patients and interventions based on AI-driven risk and utilization insights to maximize impact.
• Telehealth: Supports virtual and hybrid care delivery models, facilitating remote patient assessments, monitoring, and engagement to extend care beyond traditional settings.
• Multi-Channel Communication: Enables coordinated outreach through various channels (phone, text, email, portal) powered by AI to ensure timely and effective patient and provider engagement.
Clinical Impact:
McLaren Physician Partners reduced emergency department overutilization significantly within six months of implementing the initiative. The platform also reduces clinician documentation clicks, enabling healthcare providers to allocate more time to direct patient care activities.
ROI & Performance:
Organizations using CareSpace® experience a notable acceleration in patient revenue compared to industry averages. A recent $107 million investment underscores strong market confidence in the platform’s AI capabilities.
CareSpace® leverages machine learning algorithms to analyze patient data patterns and predict health risks. This proactive approach enables organizations to reduce 65% of hospital readmissions in 30 days while improving clinical outcomes and patient satisfaction scores across the healthcare operations.
Best For: Value-based care organizations, ACOs, and health systems participating in Medicare Shared Savings Programs that need predictive analytics for population health management and risk adjustment.
2. AthenaOne® – Cloud-Based Care Coordination Platform
AthenaOne® connects over 160,000 healthcare providers through its cloud-based ecosystem, specializing in ambulatory care coordination and revenue cycle management for independent practices and community health centers.
Key Features:
• Natural language processing for automated administrative task handling
• Integration with payer networks for real-time eligibility verification
• Telehealth platform with intelligent scheduling and automated reminders
• Mobile-first design for point-of-care access and documentation
• Cloud-based infrastructure with automatic updates and maintenance
Clinical Impact:
Healthcare practices save many hours per week through workflow automation. The telehealth integration reduces patient no-show rates through intelligent scheduling and automated patient communication systems.
Performance:
Practices increase annual patient capacity through optimized scheduling algorithms. Revenue cycle improvements lead to faster accounts receivable turnover.
Best For: Independent practices, urgent care centers, and community health centers that need cloud-based care coordination without the complexity and costs of enterprise-level platforms.
3. Cerner HealtheIntent®: Enterprise Security for Large Health Systems
Oracle’s Cerner HealtheIntent® platform processes billions of clinical transactions monthly, emphasizing security and large-scale population health management for integrated delivery networks and Medicare Advantage plans.
Security features:
• Quantum-resistant encryption for data protection
• HIPAA-compliant blockchain technology for care plan auditing
• Real-time anomaly detection enhances security by preventing numerous potential breaches annually
• Enterprise-grade disaster recovery and backup systems
Clinical impact results:
• Significant reduction in HbA1c levels for diabetic populations
• Faster sepsis identification has been reported
• Reduction in redundant medical tests
• Cost savings have been observed per member in Medicare Advantage plans
Network Connectivity:
The CommunityWorks initiative connects numerous critical access hospitals with academic medical centers, standardizing referral workflows. This network helps smaller hospitals access advanced tools typically available only to large health systems.
Performance:
The platform excels at managing chronic conditions across large patient populations through predictive analytics that identify high-risk patients before acute episodes occur.
Best for: Large health systems, integrated delivery networks, and Medicare Advantage plans requiring enterprise-grade security and comprehensive population health management tools.
Did You Know? In early 2025, Oracle Health experienced a significant data breach affecting approximately 263,000 individuals, raising concerns about its cybersecurity measures.
4. Epic Care Everywhere®: Interoperability Champion for Academic Centers
Epic dominates healthcare interoperability through its Care Everywhere network, which spans over 2,700 hospitals. The platform exchanges 24 million patient records daily, making outside medical records available in just seconds during emergencies.
Interoperability statistics:
• U.S. citizens have health data accessible through Epic’s network
• Reduction in duplicate imaging studies through centralized records
• Improvement in health equity outcomes through SDOH screening
• Acceleration in FDA drug approval processes using real-world evidence
Patient engagement:
MyChart patient portal serves millions of active users with AI-powered symptom checkers that resolve maximum patient inquiries without staff intervention. Automated prior authorization features reduce prescription abandonment, which improves medication adherence and clinical outcomes.
Research capabilities:
The Cosmos research database contains a vast amount of de-identified patient records that power clinical studies and treatment optimization algorithms. Cancer treatment response predictors achieve approximately 80% accuracy, helping oncologists make better treatment decisions.
Performance:
The platform’s strength lies in connecting large, complex health systems where seamless data sharing between departments and facilities is critical for patient safety and operational efficiency.
Best for: Academic medical centers, large health systems, and research hospitals where comprehensive interoperability and research capabilities are essential for operations and clinical trials.
5. HealthEdge GuidingCare®: Payer-Focused Administrative Automation
HealthEdge specializes in payer-centric care, serving multiple health plans and covering millions of members. The GuidingCare® platform excels at administrative automation and connecting healthcare delivery with insurance operations.
Automation capabilities:
• Authorization requests resolved in under 90 seconds using natural language processing
• HealthEdge achieves a high auto-adjudication rate for clean insurance claims
• Significant reduction in manual claim adjustments
• Reduction in out-of-network referrals through provider network analytics
Social determinants integration:
The platform integrates 1000s of community social service agencies to address social determinants of health. Housing instability interventions drive approximately a 20% reduction in emergency department visits through behavioral health coordination.
Financial performance:
Offers a competitive ROI timeline among major vendors, with notable administrative cost reduction and per-member-per-month savings. Further, the platform reduces member cost inquiries through real-time benefits verification.
Best for: Health plans, insurance companies, and payer organizations needing automated prior authorization, comprehensive member management, and streamlined administrative operations.
Integration Requirements and Technical Specifications
Healthcare IT integrations face significant challenges due to inadequate planning and unrealistic expectations. Legacy systems refuse to share data, new platforms require extensive customization, and staff training takes months while patient care suffers during transitions.
Essential technical requirements:
- HL7 FHIR compliance for seamless interoperability
- API capacity to handle peak transaction volumes without degradation
- Role-based access controls for security and compliance
- Mobile responsiveness for point-of-care access
- Disaster recovery and backup capabilities with 99.9% uptime
- Vendor support response times under 4 hours for critical issues
Implementation timeline expectations:
- Basic functionality requires 3-6 months, full optimization takes up to 12 months.
- Cloud-based platforms typically deploy faster than on-premise solutions.
- Organizations should plan for productivity adjustments during the first 90 days post-implementation.
Common integration failures:
- Data mapping errors that corrupt patient records
- Authentication problems that lock out authorized users
- Performance degradation during peak usage periods
- Compliance violations due to inadequate security configurations
- Workflow disruptions that reduce staff productivity
Strategic Selection Framework for Healthcare Organizations
Balance current needs with future growth projections. A platform perfect for today’s patient volume might fail under expansion. Enterprise-grade solutions can overwhelm smaller practices with unnecessary complexity and costs.
Primary decision factors:
- Patient population size and 5-year growth projections
- Value-based care contract participation and revenue models
- Regulatory compliance requirements (CMS, Joint Commission, state-specific)
- Existing technology infrastructure and integration constraints
- Staff technical expertise and change management capacity
- Merger and acquisition plans affecting system requirements
Market positioning considerations:
Organizations participating in Medicare Shared Savings Programs need different capabilities than those focused on commercial insurance markets. CMS quality reporting requirements continue expanding, making automated compliance features increasingly valuable for long-term success.
Vendor evaluation process:
- Include clinical staff in selection from the beginning.
- Software that works well for administrators might frustrate nurses and doctors who use it daily.
- End-user feedback during evaluation prevents costly mistakes after implementation.
Takeaway
The selection of care management software determines whether healthcare organizations will thrive or struggle over the next decade. The right platform significantly reduces administrative costs while improving patient outcomes through better coordination and predictive analytics. The wrong choice drains resources while frustrating clinical staff and patients.
Organizations achieve measurable improvements in clinical outcomes, operational efficiency, and financial performance when selecting platforms aligned with their specific needs and growth objectives. The data shows clear performance differences between vendors, with ROI timelines varying depending on implementation approach and organizational readiness.
Quick selection guide based on functional model
- AI-driven population health management: Persivia CareSpace® for value-based care organizations
- Independent practice coordination: AthenaOne® for cloud-based ambulatory care
- Enterprise security and scale: Cerner HealtheIntent® for large health systems
- Academic medical center interoperability: Epic Care Everywhere® for research and teaching hospitals
- Payer operations automation: HealthEdge GuidingCare® for health plans and insurers
Frequently Asked Questions
What is care management software?
Care management software is a digital health platform that helps healthcare providers coordinate patient care efficiently. It supports care planning, scheduling, medication management, documentation, billing, and communication among care teams, patients, and families.
What are the key features of care management software?
Key features include:
- A user-friendly interface
- EHR integration
- Care planning and scheduling
- Medication management
- Automated billing
- Patient portals
- Reporting tools
- Social determinants of health tracking
How does care management software improve patient care?
It automates administrative tasks, enables real-time data sharing, and provides predictive analytics to help care teams identify care gaps, manage chronic conditions, reduce hospital readmissions, and improve patient adherence to treatment plans.
Are these care management software HIPAA-compliant and secure?
Yes, reputable platforms use secure logins, encryption, and comply with HIPAA regulations to protect patient data privacy and security across all system interactions and data storage.
Table of Contents
