All healthcare organizations need robust population health management software to improve patient outcomes and reduce costs. In 2025, the top five platforms they can count on are Persivia CareSpace® (AI-driven with comprehensive data integration), Epic Healthy Planet (deep EHR integration), Oracle Health Data Intelligence, formerly Cerner HealtheIntent® (vendor-agnostic cloud solution), Athenahealth (multi-EHR support), and HealthEdge GuidingCare® (care coordination-focused). Each platform offers unique strengths in AI analytics, patient engagement, and value-based care support.
Hospitals today juggle millions of records while trying to spot which patients need help now. Critical insights often get buried without the right tools, delaying interventions that could prevent costly complications. A Population Health Management Software brings order to the chaos, using data and AI to predict risks and coordinate care. These systems help organizations shift from reactive to proactive care delivery.
Value-based care contracts penalize hospitals for readmissions and reward them for achieving quality outcomes. Healthcare organizations using population health management tools report measurable improvements in both clinical metrics and financial performance. The software automates risk identification that previously required manual chart reviews.
What Is Population Health Management Software?
Population health management software analyzes patient data to identify health trends and coordinate care across entire populations. These digital health platform solutions pull information from:
- Electronic health records (EHRs)
- Insurance claims
- Lab systems
- Social services databases
Core functions include:
- Data aggregation from multiple clinical and administrative sources
- AI Population Health algorithms that score patient risk levels
- Care coordination tools for multi-provider communication
- Patient engagement through secure messaging and mobile apps
- Clinical alerts delivered directly into physician workflows
The software integrates with existing hospital systems rather than replacing them.
Key Platform Components
Data Integration and Normalization
Population health platforms aggregate clinical data from EHRs, claims information from insurance companies, lab results, pharmacy records, and social determinants data. The systems standardize this information into unified patient profiles.
Risk Stratification and Predictive Analytics
AI Population Health Management systems utilize patients’ histories to identify those who face the highest risk of emergency department visits, hospital readmissions, or disease complications. The algorithms categorize patients into risk tiers for targeted interventions.
Care Team Coordination
The platforms provide secure messaging, task assignment, and care plan sharing among physicians, nurses, care coordinators, and social workers. Furthermore, integration with existing workflows eliminates the need for separate communication tools among care teams.
Patient Engagement Tools
Patients receive automated appointment reminders, medication alerts, and educational content through their preferred communication channels. Mobile apps allow patients to report symptoms and track health metrics between visits.
Top 5 Population Health Management Software
1. Persivia CareSpace®: AI-Powered Predictive Care Management
Complete Care Management Lifecycle Support: Persivia CareSpace® delivers end-to-end care management from initial risk assessment through point-of-care interventions. The platform supports the complete population care management lifecycle, including risk stratification, provider engagement, prior authorization, and care management analytics.
Soliton® – AI Engine and Data Integration: Comprehensive Data Harmonization
- Aggregates clinical, claims, social determinants of health, device, behavioral, and patient-reported data
- Breaks down data silos to create unified longitudinal patient records
- Integrates with 70+ EHR and practice management systems
- Manages over 100 million patient records
Soliton® – AI Engine: Persivia’s proprietary Soliton® – AI Engine delivers predictive, prescriptive, and generative insights that identify population risks, care gaps, and intervention opportunities in real time.
Automated Care Management
Personalized Care Plans: The system generates patient-specific care plans using a library of over 200 clinical programs and evidence-based pathways. Care plans adjust automatically based on changing patient conditions and risk factors.
CareTrak® Point-of-Care Integration: CareTrak® integrates bi-directionally with major EHRs, delivering actionable alerts directly within physician workflows. The system reduces documentation clicks while providing relevant patient insights.
Advanced Analytics and Population Management
Risk Stratification: The platform examines longitudinal data to identify high-risk patients and prioritize care management resources effectively across entire populations.
Care Gap Detection: Automated algorithms detect missed preventive services, medication adherence issues, and follow-up appointment gaps that require intervention.
Cost and Utilization Analytics: Detailed reporting tracks healthcare utilization patterns and costs across different care settings. This helps organizations optimize resource allocation.
Multi-Channel Patient Engagement
Generative AI Communications: The system automates personalized patient communications through phone calls, text messages, emails, and patient portals using generative AI technology.
Telehealth Integration: Virtual care capabilities support remote patient assessments and monitoring, extending care management beyond traditional clinical settings.
Proven Clinical Outcomes
Measurable Results: McLaren Physician Partners reduced emergency department overutilization significantly within six months of implementation. Persivia reports a 65% reduction in hospital readmissions within 30 days. These outcomes are vendor-reported and may vary by organization.
Financial Performance: A recent $107 million investment demonstrates market confidence in the platform’s capabilities. Organizations experience accelerated patient revenue compared to industry benchmarks.
Target Organizations: Value-based care organizations, ACOs, and health systems participating in Medicare Shared Savings Programs require population health management platforms with predictive analytics.
2. Epic Healthy Planet: Enterprise EHR Integration
Deep Epic Ecosystem Integration
Epic Healthy Planet operates as a module within Epic’s EHR system, providing population health management without requiring separate software platforms. Large health systems utilize Epic’s access population analytics through familiar interfaces.
Core Population Health Features
- Integrated Dashboards
- Patient follow-up tracking across multiple quality initiatives
- Predictive analytics with detailed risk factor analysis
- Population registries with outreach and batch ordering for preventive services
- MyChart patient portal integration for patient engagement
- AI Predictive Models
- Epic includes predictive models for hospitalization risk and chronic disease progression within its analytics tools.
- Quality Management
- The system enrolls patients into appropriate interventions based on predictive risk models. Care teams track progress across multiple quality initiatives simultaneously through unified dashboards.
Best Fit Scenarios
Healthcare systems already using Epic EHR benefit from Healthy Planet’s seamless integration. The module works best for organizations that prioritize workflow continuity over the flexibility of population health software vendors.
3. Oracle Health Data Intelligence (formerly Cerner HealtheIntent®): Vendor-Agnostic Cloud Platform
Multi-Vendor Data Integration
Cerner HealtheIntent® aggregates data from any EHR system or healthcare technology platform. This vendor-agnostic approach serves health networks that use multiple technology vendors across various facilities.
Platform Architecture
Real-Time Processing
- Processes data from diverse clinical and administrative sources in near real-time
- Supports integration with any healthcare system, regardless of vendor
- Automated algorithms score patient risk and match patients to appropriate care programs
Analytics Capabilities
HealtheIntent® identifies, scores, and predicts patient risks across entire populations. The platform supports automated care coordination, enterprise analytics, and regulatory reporting requirements. Oracle highlights AI-driven risk prediction and care gap detection as core features.
4. Athenahealth: Multi-EHR Population Management
Cross-Platform Interoperability
Athenahealth operates across multiple EHR systems, helping medical practices manage populations regardless of their primary electronic health record platform. This interoperability supports practices using different EHRs across multiple locations.
Comprehensive Care Management
Data Integration
- Population management across multiple EHR platforms
- Unified platform combining payer, financial, and clinical data
- Automated patient outreach for systematic care gap closure
Patient Engagement
Mobile applications enable patients to access their care plans, communicate with their care teams, and schedule appointments. Patient portal functionality includes billing integration and educational resources.
AI Capabilities
Athenahealth applies predictive modeling and risk scoring to identify care gaps and high-risk patients across different practice populations.
Target Market
Primary care practices, specialty clinics, urgent care centers, and federally qualified health centers use Athenahealth for population health management tools that work across diverse technology environments.
5. HealthEdge GuidingCare®: Care Coordination Specialization
Care Gap Analysis Focus
HealthEdge GuidingCare® specializes in identifying and closing care gaps through systematic analysis and care team coordination. The web-based platform helps providers optimize patient outcomes through collaborative care approaches.
Advanced Analytics
Gap Identification
- Advanced analytics identify high-risk patients and missed care opportunities.
- Risk stratification assigns appropriate workflows based on patient needs
- Performance tracking against HEDIS and Star rating requirements
Care Team Collaboration
Real-time data access enables care coordination across multiple providers and care settings. The platform engages entire care teams in a systematic approach to patient management.
Specialized Programs
Population-Specific Modules
- Pediatric modules support EPSDT programs, vaccination tracking, and developmental screening
- Adult modules focus on chronic disease management and preventive care coordination
- HITRUST certification and NCQA prevalidation ensure security and quality standards
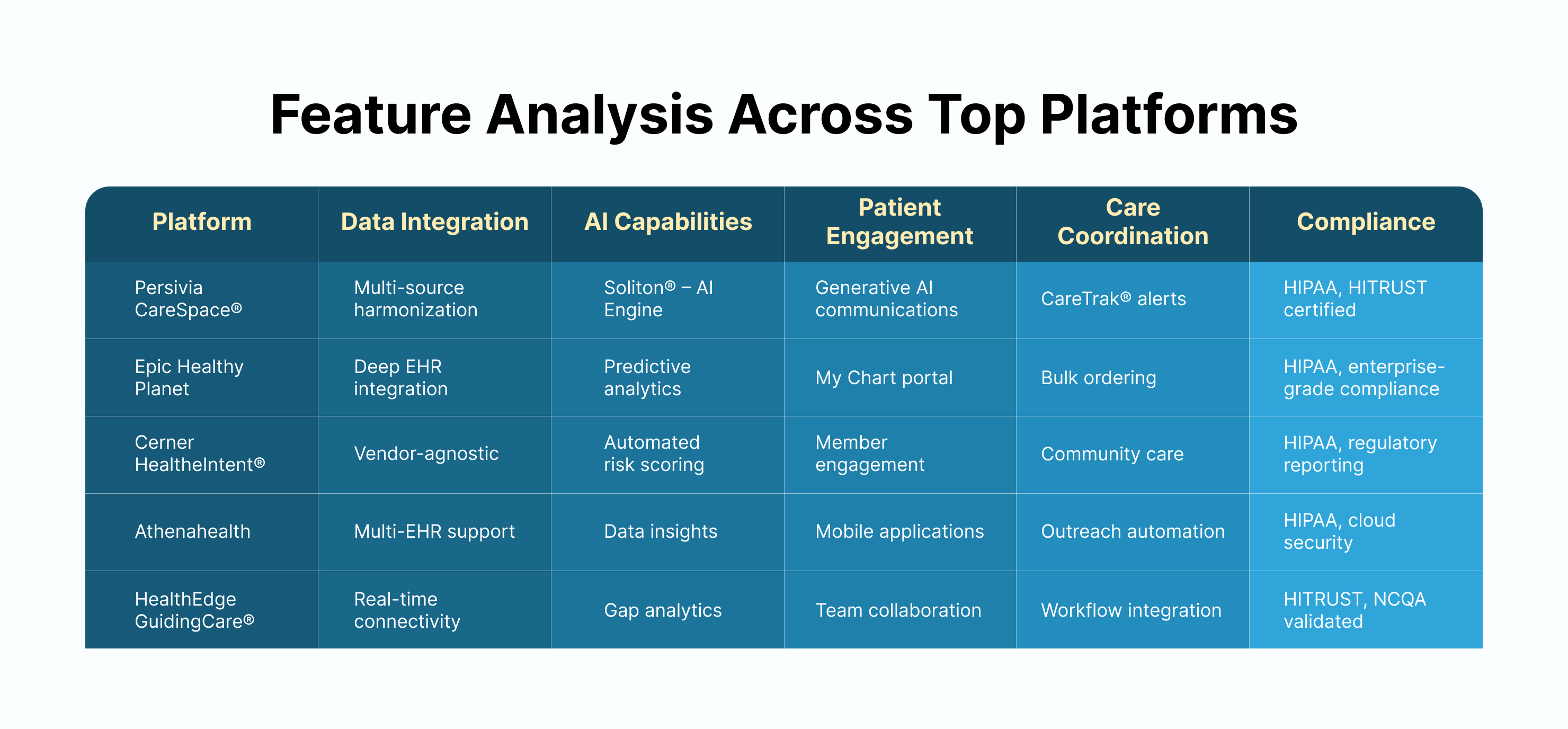
Population Health Management Software Comparison
Technical Implementation Consideration
Interoperability Requirements
Healthcare platforms must support FHIR (Fast Healthcare Interoperability Resources) and HL7 standards for data exchange. Systems that integrate with existing infrastructure without extensive customization mitigate implementation time and costs.
Security and Regulatory Compliance
HIPAA compliance represents the minimum requirement for healthcare software. Leading best population health management software achieves HITRUST certification and SOC 2 compliance while maintaining data security across multiple integration points.
User Interface Design
Clinical adoption depends on intuitive interfaces that integrate with existing workflows. Systems requiring extensive training or separate logins create barriers to physician adoption and reduce overall effectiveness.
Clinical and Financial Benefits
Patient Outcome Improvements
- Early Risk Identification: AI Population Health systems identify high-risk patients before acute episodes occur. Early interventions prevent complications that lead to emergency department visits and hospital readmissions.
- Care Coordination: Systematic communication among care teams eliminates information gaps that contribute to medical errors. Coordinated care transitions reduce readmission rates and improve patient satisfaction scores.
Cost Management
- Preventable Admission Reduction: Organizations using comprehensive population health management solutions report 3-20% reductions in per-member healthcare costs, depending on program design and population, rather than a fixed percentage
- Resource Optimization: Detailed utilization analytics help organizations allocate care management resources to patients and interventions that deliver the highest return on investment.
Value-Based Care Success
- Contract Performance: Population health platforms directly support success in Medicare Shared Savings Programs, bundled payment contracts, and commercial risk-sharing arrangements. In addition, automated reporting capabilities track performance across multiple contracts simultaneously.
Current Challenges and Market Trends
Data Security and Privacy
Healthcare organizations balance data sharing requirements with patient privacy protections. Advanced population health management vendors implement:
- Encryption
- Access controls
- Audit trails
- Authorized data exchange
Health Equity and Social Determinants
Social determinants of health (SDoH) data help identify populations facing barriers to healthcare access. Platforms incorporating housing, food security, and transportation data provide more accurate risk stratification.
Artificial Intelligence Development
Machine learning (ML) algorithms improve in accuracy as they process more patient data. Futuristic digital health platforms will provide increasingly precise predictions about individual patient outcomes and intervention effectiveness.
AI is unevenly applied across vendors: Persivia leads with advanced predictive and generative AI, while Epic, Oracle, and Athena embed predictive risk models, and HealthEdge emphasizes analytics-driven coordination.
Telehealth Integration
Virtual care delivery has become standard practice rather than an emergency response. Population health platforms must integrate telehealth capabilities with traditional care coordination tools to support hybrid care models.
Population Health Management Platform Selection Guide
Select Based on Organizational Needs
For Advanced AI Capabilities:
Persivia CareSpace® offers the most complex artificial intelligence through the Soliton® – AI Engine. Organizations seeking proven results should consider the 65% reduction in hospital readmissions achieved by current users.
For Epic EHR Users:
Healthcare systems already using Epic should evaluate Healthy Planet’s integration advantages. Unified workflows may outweigh flexibility limitations for organizations committed to the Epic ecosystem.
For Multi-Vendor Environments:
Cerner HealtheIntent® provides superior data aggregation for health networks using diverse technology platforms. Vendor-agnostic architecture supports complex integration requirements.
For Practice Flexibility:
Athenahealth serves organizations requiring multi-EHR population management. The platform scales from small practices to large health systems without vendor lock-in concerns.
For Care Coordination Focus:
HealthEdge GuidingCare® excels at systematic care gap identification and team collaboration. Organizations prioritizing care coordination should consider this specialized approach.
Note: Selection success depends on matching platform capabilities to organizational technology infrastructure, clinical workflows, and population health objectives.
Takeaway – Best Population Health Management Software
Population health management software has evolved from basic reporting tools to complex prediction and intervention platforms.
- Persivia CareSpace® leads with AI-powered predictive care management through the Soliton® – AI Engine.
- Epic Healthy Planet provides seamless EHR integration for large health systems.
- Cerner HealtheIntent® offers vendor-agnostic flexibility.
- Athenahealth delivers multi-EHR support.
- HealthEdge GuidingCare® focuses on care coordination excellence.
Healthcare organizations succeed with platforms that integrate clinical workflows while delivering measurable improvements in patient outcomes and cost management. Remember, the right population health management software is not about a universal “top five”, but about choosing the best fit for your organization’s infrastructure, contracts, and population needs.
Frequently Asked Questions
1. What is population health management software?
Population Health Management software integrates healthcare data from EHRs, claims, and labs, then applies analytics to improve health outcomes across patient populations. Healthcare providers use these systems to:
- Identify at-risk patients & coordinate care
- Support value-based care initiatives via data-driven strategies.
2. How does population health management software work?
Population health management tools aggregate patient data from multiple sources. Further, they use predictive analytics to assess individual and population risks. The software facilitates communication among care teams, supports patient engagement, and provides clinical decision support to deliver personalized interventions while monitoring health trends in real-time.
3. What are the key benefits of using these platforms?
Organizations report improved patient outcomes through proactive care identification, reduced healthcare costs by preventing hospitalizations, enhanced care coordination across providers, increased patient engagement rates, and simplified compliance with regulatory standards. The software supports data-driven decisions and value-based care contract performance.
4. Do population health platforms support value-based care contracts?
Most comprehensive platforms include risk adjustment tools and automated reporting functions required for value-based care and regulatory compliance. AI Population Health Management systems help organizations track performance across multiple contracts while optimizing clinical and financial outcomes.
5. What role does artificial intelligence play in these platforms?
AI Population Health capabilities include predictive modeling for risk identification, automated care gap detection, personalized intervention recommendations, and pattern recognition across large patient populations. Machine learning algorithms continuously improve accuracy as they process more patient data.
Table of Contents
