The 2026 CMS TEAM Model launched January 1. Right now, 741 hospitals are operating under a completely different payment structure for surgical care.
For those hospitals, the first month has been a learning experience. The Transforming Episode Accountability Model is a fundamental shift in how Medicare pays for major surgical procedures, with real financial risk.
CMS states the model aims to improve health outcomes by “holding participants accountable for all the costs of care for an episode” which “incentivizes care coordination, can improve patient care transitions, and decreases the risk of avoidable readmission.” More information is available on the official CMS TEAM Model page.
What is new in 2026 CMS TEAM Model?
The CMS TEAM Model is a mandatory, five-year bundled payment program that launched January 1, 2026, and runs through December 31, 2030. Instead of separate service payments, hospitals receive a target price for an entire episode of care covering 30 days post-discharge.
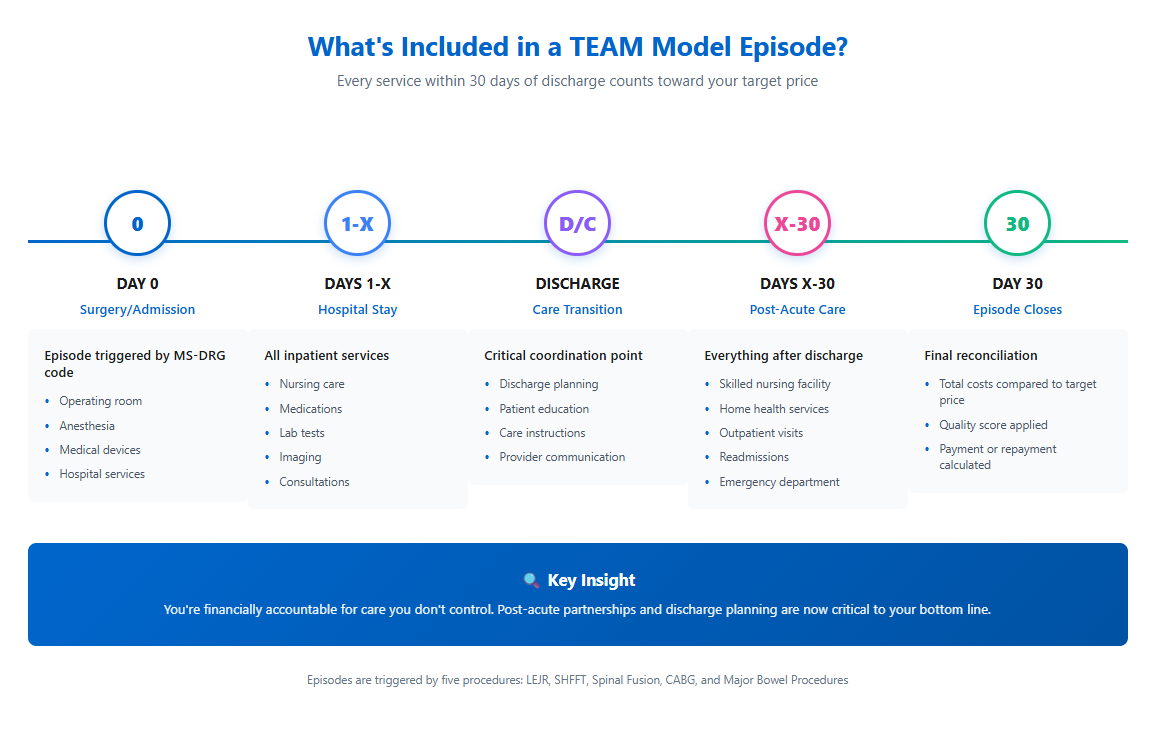
The model covers five procedures: Lower Extremity Joint Replacement (LEJR), Surgical Hip/Femur Fracture Treatment (SHFFT), Spinal Fusion, Coronary Artery Bypass Graft (CABG), and Major Bowel Procedures. Episodes are triggered by specific MS-DRG and HCPCS billing codes.
Hospitals still bill Medicare fee-for-service. But at year-end, CMS reconciles actual spending against target prices. According to CMS, “TEAM participants may earn a payment from CMS, subject to a quality performance adjustment, if the total Medicare costs for the episode are below the target price. TEAM participants may owe CMS a repayment amount, subject to a quality performance adjustment, if the total Medicare costs for the episode are above the target price.”
The model covers five procedures: Lower Extremity Joint Replacement (LEJR), Surgical Hip/Femur Fracture Treatment (SHFFT), Spinal Fusion, Coronary Artery Bypass Graft (CABG), and Major Bowel Procedures. Episodes are triggered by specific MS-DRG and HCPCS billing codes.
Hospitals still bill Medicare fee-for-service. But at year-end, CMS reconciles actual spending against target prices. According to CMS, “TEAM participants may earn a payment from CMS, subject to a quality performance adjustment, if the total Medicare costs for the episode are below the target price. TEAM participants may owe CMS a repayment amount, subject to a quality performance adjustment, if the total Medicare costs for the episode are above the target price.”
CMS projects $481 million in Medicare savings over five years. projects $481 million in Medicare savings over five years.
Who Are the 2026 CMS TEAM Model Participants?
CMS released the mandatory participant list September 5, 2024: 741 acute care hospitals across 188 Core-Based Statistical Areas nationwide.
Participation isn’t voluntary. Hospitals paid under IPPS in a selected CBSA must participate. Maryland hospitals and Critical Access Hospitals are excluded. The official CMS TEAM participant list allows verification by hospital name or CCN.
CMS TEAM Model Quality Measures: How Performance Gets Scored
The Composite Quality Score (CQS) can adjust reconciliation payments by up to 20% (from -10% to +10%). A hospital saving $200,000 against target could receive $220,000 with a +10% adjustment or only $180,000 with a -10% adjustment.
Three quality measures determine Performance Year 1 scores:
Hybrid Hospital-Wide Readmission (HWR)
30-day readmissions using claims and EHR data.
Patient Safety Indicator 90 (PSI 90)
Adverse events like infections, pressure ulcers, and falls.
THA/TKA PRO-PM
Joint replacement patient-reported outcomes on pain and function.
Scoring gets weighted by episode volume. Performance Year 3 adds the Information Transfer PRO-PM. Full details in the CMS TEAM Quality Measures document.
Key Updates from the 2026 CMS TEAM Model Final Rule
CMS published the final rule on July 31, 2025. Key updates:
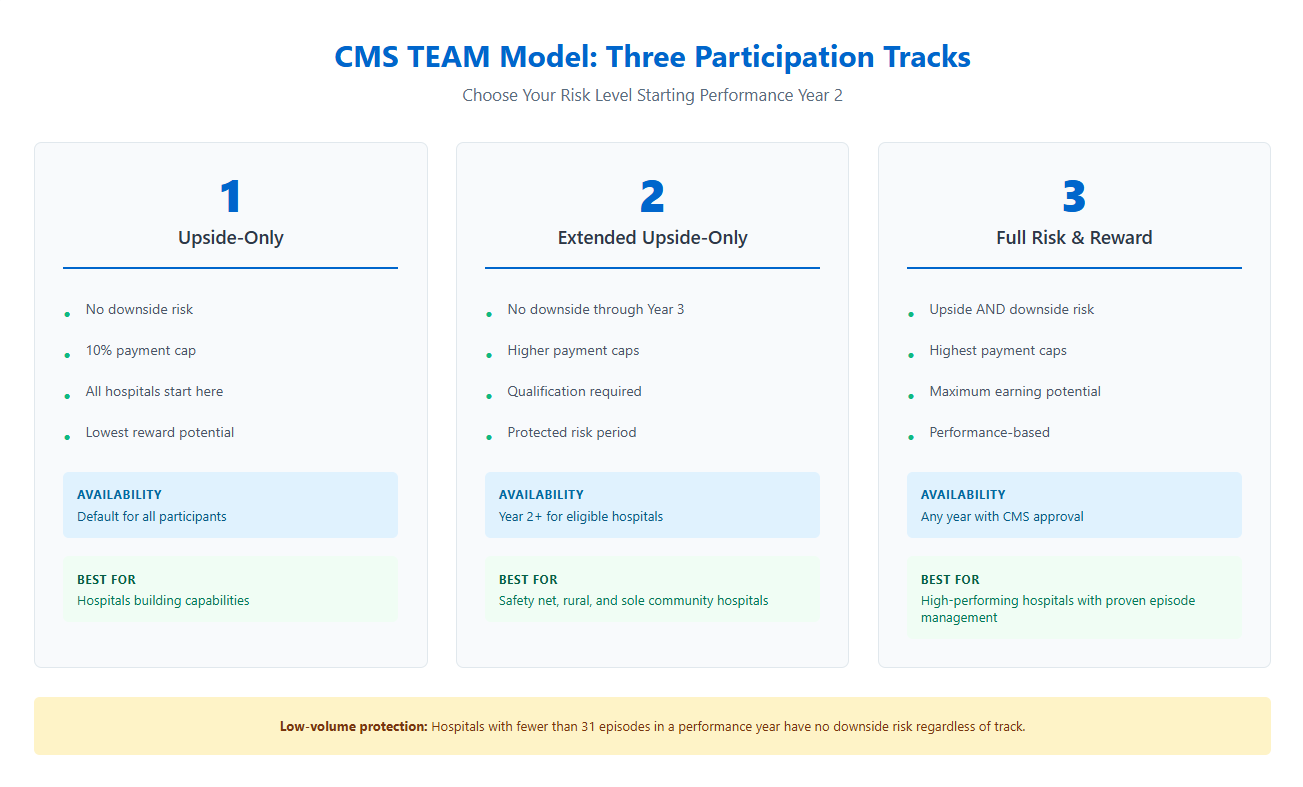
Three-Track Participation System:
- Track 1: Upside-only, no downside risk, 10% cap. All hospitals start here.
- Track 2: For safety net, rural, and sole community hospitals starting Year 2.
- Track 3: Full risk and reward with higher caps. Available any year.
Hospitals not selecting a track get placed in Track 1 automatically. Low-volume protection applies to fewer than 31 episodes means no downside risk.
Risk Adjustment
Target prices account for patient factors (age, HCC count, social risk) and hospital factors (bed size, safety net status, teaching designation), leveling the playing field for hospitals serving complex populations.
Target prices use regional spending data adjusted for risk factors and demographics. CMS applies discount factors of 1.5% (CABG, bowel) and 2% (other procedures).
What Hospitals Should Focus on in Performance Year 1 (2026)
Performance Year 1 offers a unique opportunity. All hospitals start in Track 1 with upside-only risk. There’s no downside financial risk in 2026, but the actions hospitals take this year will determine success in Years 2-5.
2026 Action Plan: Building While the Stakes Are Low
When CMS Releases First Monthly Claims Data This Month
CMS released baseline data and target prices in Fall 2025. Now, with Performance Year 1 underway, February 2026 brings the first monthly claims data showing actual episode performance. When this live data arrives, hospitals need to immediately:
- Analyze actual episode spending against target prices to identify which procedures are trending over or under budget
- Review episode volume to confirm all TEAM-eligible cases are being captured and no episodes are missing from reports
- Assess which providers and care patterns are driving high-cost episodes and where intervention is needed
Then build the infrastructure. Since there’s no downside risk this year, use 2026 to test and refine:
Episode Management: Implement real-time visibility into episode costs as they accumulate. Don’t wait until reconciliation in 2027 to discover you’re spending over target.
Quality Monitoring: Establish dashboards for the three quality measures (HWR, PSI 90, PRO-PM). Your Composite Quality Score directly impacts financial outcomes starting Year 1.
Care Coordination: Strengthen discharge planning and post-acute provider relationships. The 30-day accountability window means skilled nursing facilities and home health agencies are now part of your financial picture.
Post-Acute Partnerships: Identify SNFs with strong outcomes and lower costs. Develop preferred home health partnerships with clear communication protocols. Create pathways for patients who can safely discharge directly home.
Data Integration: Connect hospital, SNF, home health, and outpatient data streams so you can see the full 30-day episode cost in real time.
Clinical Engagement: Share target price data with surgeons, hospitalists, care managers, and discharge planners. They need to understand how clinical decisions affect financial outcomes.
Prepare for Track Selection in 2027
While 2026 has no downside risk, hospitals must choose a track for Year 2: Stay in Track 1 to avoid risk, move to Track 3 if performance shows consistent savings, or qualify for Track 2 if you’re a safety net, rural, or sole community hospital.
How Persivia Supports Success in the 2026 CMS TEAM Model
The CMS TEAM Model requires infrastructure that most hospitals don’t have ready. Real-time episode tracking, cost monitoring, quality measure capture, risk adjustment optimization, and seamless care coordination workflows.
Persivia’s CareSpace® platform is built specifically for value-based care models like CMS TEAM. Episode analytics show which cases are trending over target while intervention is still possible. The platform’s AI-powered risk adjustment tools accurately capture HCC codes and provide real-time risk stratification, ensuring hospitals maximize their risk-adjusted target prices.
Quality measure tracking is built into workflows, with patient-reported outcomes collected at the right times and readmission risk flagged early. Intuitive dashboards monitor HCC capture and recapture rates, critical for optimizing risk adjustment performance. Advanced data integration ensures accurate MS-DRG and HCPCS code tracking for all TEAM-eligible episodes.
The care coordination module connects hospital teams with post-acute providers, giving discharge planners visibility into skilled nursing facility capacity and outcomes. Persivia supports all three participation tracks and integrates seamlessly with existing EHR systems.
What Success Looks Like by December 2026 CMS TEAM
Successful hospitals will have accurate episode tracking, real-time cost monitoring, quality performance at national benchmarks, HCC capture rates above 90%, established post-acute networks, and care coordination workflows connecting patients to primary care.
The first reconciliation won’t be calculated until mid-2027, but hospitals building these capabilities now will earn shared savings while others struggle.
Frequently Asked Questions About the 2026 CMS TEAM Model
When does the CMS TEAM Model start? It launched January 1, 2026, and runs five years through December 31, 2030.
Which hospitals must participate? 741 acute care hospitals in 188 selected CBSAs. Check the CMS official list.
What are the quality measures? Hospital-wide readmission, PSI 90 patient safety, and THA/TKA patient-reported outcomes.
Can hospitals avoid downside risk? Track 1 has no downside in Year 1. Safety net hospitals extend that through Year 3.
Conclusion – 2026 CMS TEAM
The CMS TEAM Model is now active, and 2026 is your strategic opportunity. With Track 1’s upside-only risk, hospitals can build episode management capabilities without downside financial exposure.
With the first monthly performance data arriving this month, successful hospitals will immediately analyze actual spending patterns, identify episodes trending over target, and intervene before losses accumulate. They’ll use real-time insights to refine care pathways and post-acute strategies. The hospitals that treat 2026 as a learning year will regret it when reconciliation arrives. The hospitals that treat it as a building year will thrive.
See how Persivia helps hospitals track episodes in real time, optimize risk adjustment, and coordinate care across the full 30-day accountability window. Request a Demo.
Table of Contents
