The Evolution of Healthcare: From Fee-for-Service to Value-Based Care
The US healthcare landscape is undergoing a fundamental transformation. Organizations across the country are shifting away from the traditional fee-for-service (FFS) model—where providers are paid based on the quantity of services delivered—toward value-based care (VBC) models that prioritize quality outcomes over volume. This paradigm shift represents more than just a change in payment structure; it’s a complete reimagining of how healthcare is delivered, measured, and improved.
At the heart of this transformation lies population health management—a strategic approach that has become essential for healthcare organizations navigating the transition to value-based care. Population health management enables providers to look beyond individual patient encounters and address health outcomes across entire communities, creating opportunities for more efficient resource allocation and better overall outcomes.
What is Population Health Management?
Population health management aims to improve the overall health of a group of people. It works by identifying cohorts with similar traits, health conditions, economic circumstances, or social factors, and then applying targeted interventions designed specifically for each group’s needs.
Rather than treating each patient individually, population health management recognizes patterns across groups and implements strategies that address both individual and collective needs. This approach includes:
• Stratifying populations based on risk and health status
• Creating tailored intervention programs for specific segments
• Connecting patients with appropriate clinical and social services
• Continuously monitoring outcomes and adjusting approaches
• Leveraging preventive care to maintain wellness before problems escalate
By addressing the unique needs of each population segment while applying consistent approaches across similar groups, healthcare organizations can improve health outcomes for entire communities more efficiently.
Clinical Programs: The Engine of Population Health Management
At the heart of effective population health management lies clinical programs—structured, evidence-based frameworks designed to address specific health challenges across defined patient populations. These programs transform basic population health concepts into practical, actionable workflows.
How Clinical Programs Organize Patient Populations
Clinical programs work by categorizing patients into distinct “buckets” based on shared characteristics, allowing for targeted interventions across similar populations.
The categorization process typically works through several layers:
- Primary Segmentation by Clinical Profile: Patients are first grouped by clinical conditions such as diabetes, heart failure, COPD, or hypertension. This creates foundational segments of patients who share core medical needs.
- Risk Level Stratification: Within each clinical segment, patients are further divided by risk levels, identifying those at high risk for complications or hospitalization versus those who are stable but require ongoing management.
- Care Gap Analysis: Populations are assessed for specific care gaps such as missed screenings, overdue follow-ups, or unmet preventive care needs.
- Behavioral and Adherence Patterns: Programs identify patients with similar challenges in medication adherence, appointment attendance, or self-management behaviors.
- Social Determinant Clustering: Patients facing similar social and economic barriers—such as transportation limitations, food insecurity, or housing instability—are grouped to enable coordinated interventions.
For example, a diabetes management program might create distinct patient buckets for:
• Newly diagnosed patients requiring education and initial management
• Patients with uncontrolled diabetes and high A1C levels needing intensive intervention
• Well-controlled diabetics requiring maintenance monitoring
• Diabetics with social determinant barriers affecting their self-management capabilities
• Diabetics with multiple comorbidities requiring complex care coordination
Once patients are categorized into these distinct population groups, they are enrolled into specific programs to address their unique needs.
The Critical Role of Data and Longitudinal Patient Records
The transformative potential of clinical programs begins with data. Without comprehensive, integrated information, even the most sophisticated AI systems cannot deliver meaningful insights.
Longitudinal patient records—which capture the complete health journey of each individual across time and care settings—form the foundation of effective population health management. These unified records integrate data from disparate sources to create a comprehensive view of each patient’s health status, history, and needs.
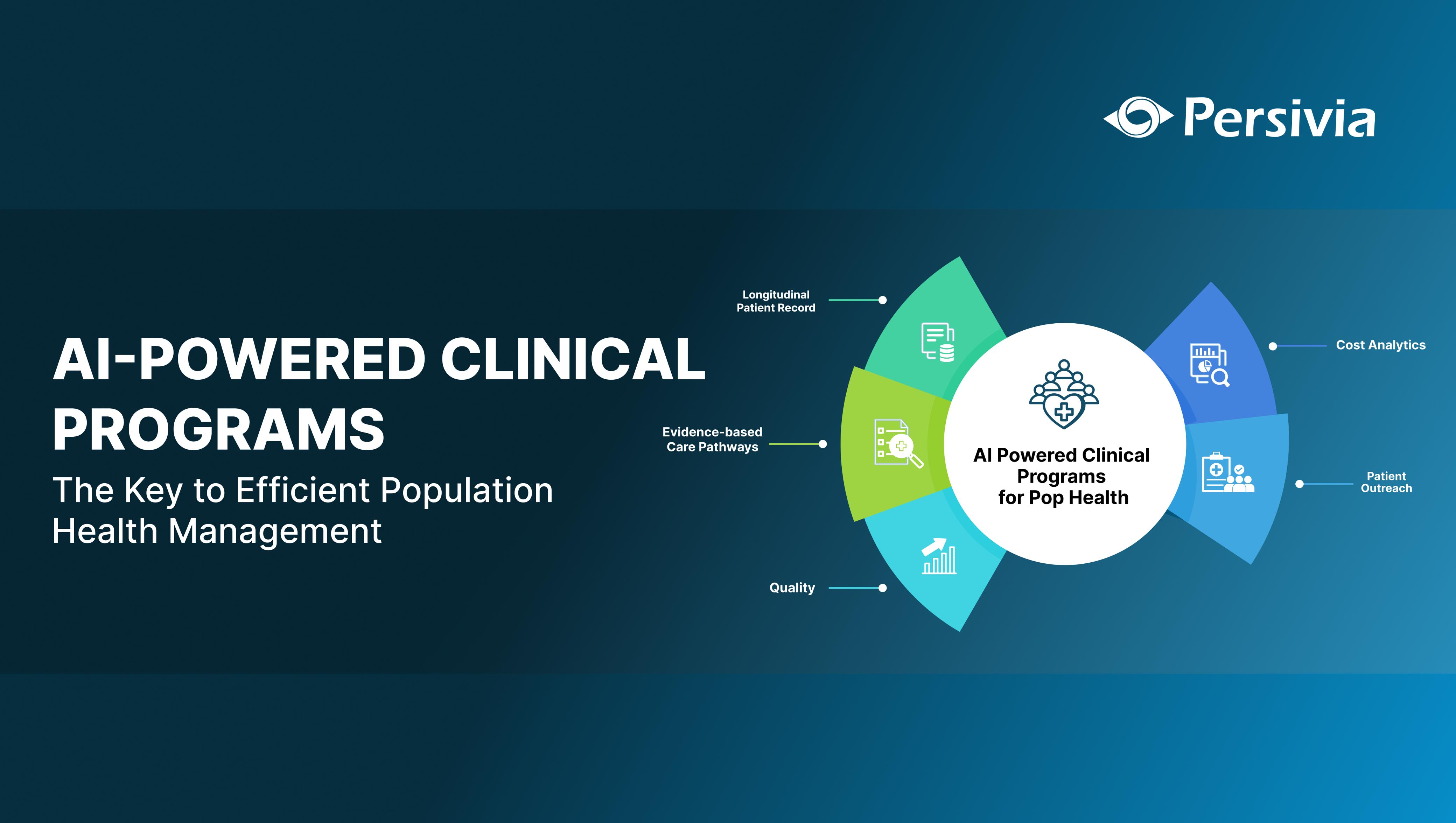
Persivia’s AI-Driven Clinical Programs: The Next Generation Population Health Management
1. It Begins with Data Integration
At the heart of Persivia’s approach lies data integration—the most critical element of effective population health management. Persivia’s CareSpace® aggregates information from all disparate sources including EMRs, EHRs, claims data, lab results, patient-reported data, device data, and social determinants of health.
This comprehensive data integration creates a single longitudinal patient record that provides care teams with a complete picture of each patient’s health journey. Unlike fragmented approaches that miss critical connections, this unified view enables providers to make informed decisions quickly and accurately, identifying subtle patterns that might otherwise go unnoticed.
2. Powering Intelligence Through AI
With this integrated data foundation, Persivia leverages sophisticated AI and rules engines to segment populations based on precise clinical indicators. The system continuously analyzes real-time data to identify key factors such as:
• Chronic disease status and progression
• Risk scores for readmission or complications
• Open care gaps and preventive service needs
• Medication adherence patterns
• Social determinants affecting health outcomes
This intelligent analysis automatically categorizes patients into the most appropriate AI-driven clinical programs from Persivia’s extensive portfolio, which includes:
• CMS Programs like Frequent Flyers (FF), Annual Wellness Visits (AWVs), Chronic Care Management (CCM), and Transitional Care Management (TCM)
• Chronic care management for 55+ conditions
• Quality and compliance programs supporting MIPS, HEDIS, ACO requirements
3. Delivering Personalized Care Pathways
For each patient enrolled in a program, CareSpace® generates personalized clinical pathways that guide care delivery. These pathways are not static protocols but dynamic roadmaps that evolve with each patient’s health journey, ensuring interventions remain relevant and effective as conditions change.
Care teams receive these insights directly through CareTrak®, Persivia’s point-of-care tool that integrates seamlessly into existing clinical workflows. By presenting the right information at the right time, the system ensures that care teams can immediately act on program recommendations without disrupting their existing processes.
The Future of Population Health Management
The future of population health management lies in AI-driven clinical programs. By automating patient stratification, program enrollment, and care coordination, these programs enable healthcare organizations to:
- Maximize the impact of limited clinical staff
- Deliver proactive rather than reactive care
- Improve clinical outcomes while reducing costs
- Ensure consistent, evidence-based care delivery
As healthcare continues its shift from volume to value, the precision approach to population health enabled by AI-driven clinical programs becomes increasingly critical. This intelligent approach allows organizations to simultaneously improve quality metrics, enhance patient experiences, and control costs across diverse patient populations.
The future of population health is here today. The question is: Will your organization be part of it?
Table of Contents