Introduction: The Value-Based Care Challenge
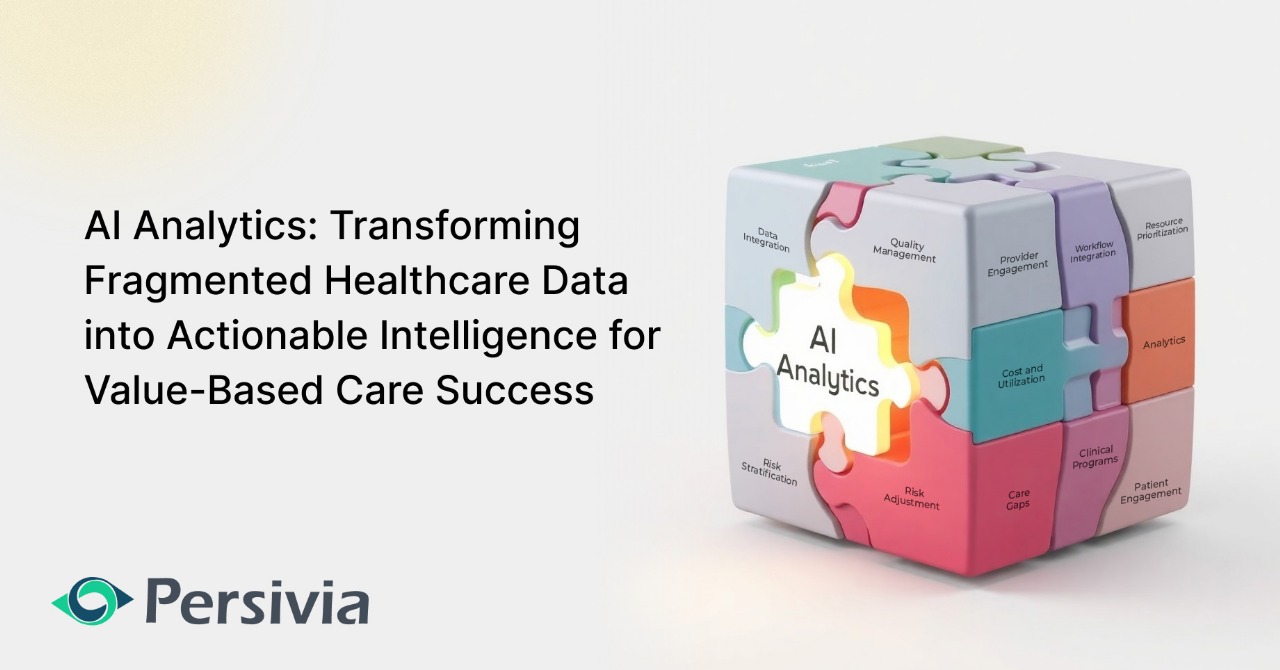
Healthcare’s equation seems straightforward: deliver better care at lower costs. Yet despite significant investments in value-based care (VBC) models, the industry continues to struggle with achieving this seemingly simple goal. The fundamental promise of VBC—improving care quality while reducing expenses by paying providers prospectively based on outcomes rather than retrospectively for each service—remains largely unfulfilled. AI-enabled value-based care analytics represents the critical missing element in this equation, offering healthcare organizations the capability to transform vast amounts of fragmented data into actionable intelligence that can finally bridge the gap between VBC’s theoretical promise and practical implementation.
The Data Foundation Problem
At the core of VBC’s challenges lies a fundamental data problem. Provider networks struggle with fragmented data systems, limited interoperability between clinical and financial information, and analytics tools that fail to deliver truly actionable insights. As VBC models evolve—spanning everything from population-based attribution to episode-specific care pathways—the ability to transform diverse healthcare data into strategic intelligence has become essential for survival.
The existing data analytics reporting infrastructure simply cannot support the sophisticated decision-making required for network optimization, quality improvement, and financial sustainability. Traditional analytics approaches leave healthcare organizations drowning in information while starving for insight.
AI-Enabled Value-Based Care Analytics: The Transformative Opportunity
Artificial intelligence (AI) represents a transformative opportunity to address these challenges. Implementation of strategic AI tools can transform VBC from a fragmented, underperforming system into a streamlined, results-driven model. Predictive analytics powered by AI helps providers transition from reactive care to proactive population health management. By analyzing patterns in patient data, AI can anticipate future health issues, enabling early intervention for chronic diseases.
AI-enabled analytics changes healthcare decision-making by revealing insights that would remain hidden otherwise. These systems can process vast datasets spanning millions of patient encounters to identify subtle correlations between seemingly unrelated factors—medication adherence patterns, socioeconomic variables, and clinical indicators—creating a multidimensional view of patient risk that far exceeds traditional risk stratification methods. This enhanced perspective allows providers to deploy personalized interventions that address not only immediate clinical needs but also underlying factors that influence health outcomes.
Beyond individual patient care, AI analytics provides healthcare organizations with system-level intelligence critical for value-based care success. By continuously learning from outcomes data, these platforms can identify optimal care pathways that balance clinical effectiveness with resource utilization, recommend evidence-based protocol adjustments in real-time, and forecast population health trends with increasing accuracy over time. This combination of micro and macro insights creates a feedback loop of continuous improvement that aligns perfectly with the core principles of value-based care: better outcomes at lower costs with improved patient experience.
Building the Right Value-Based care analytics Foundation
Effective AI analytics in healthcare doesn’t start with algorithms—it starts with data integration. Creating a unified data foundation that brings together clinical, claims, and administrative information is the essential first step toward actionable intelligence.
Persivia’s CareSpace® tackles healthcare’s data fragmentation challenge through its comprehensive Unified Data Model (UDM), which seamlessly integrates data from EHRs, claims systems, labs, social determinants of health, and hundreds of other sources. Built on the HL7 V3 Reference Information Model and fully compliant with USCDI interoperability standards, this platform creates a unified, longitudinal patient record that provides complete visibility for providers while maintaining the highest standards of data integrity.
The platform’s sophisticated data fabric transforms both structured and unstructured information into actionable intelligence, directly connecting analytics to care management workflows for immediate intervention. CareSpace® empowers organizations to identify high-risk patients earlier through its analytics engine processing millions of patient encounters, continuously optimize quality measures across value-based care models, and leverage its healthcare-optimized columnar OLAP database to understand referral patterns and provider performance variations—ultimately enabling healthcare leaders to make strategic decisions that simultaneously improve clinical outcomes and financial performance.
Conclusion
As the Centers for Medicare and Medicaid Services reports a 25% increase in VBC model participation from 2023 to 2024—including Managed Care Organizations, Accountable Care Organizations, and Medicare Advantage—the need for effective analytics solutions has never been greater.
Organizations that succeed in the evolving VBC landscape will be those that build robust data foundations, implement AI-enabled analytics, and create seamless workflows that translate insights into clinical action. By addressing the fundamental data challenges that have historically limited healthcare analytics, these organizations can finally realize the original promise of value-based care: better outcomes at lower costs.
The equation may be simple, but the execution requires sophisticated tools. AI-enabled analytics isn’t just a nice-to-have technology—it’s the missing piece that can finally make value-based care transformation possible.
Table of Contents