The CMS MSSP 2026 proposed rule is transforming the Medicare Shared Savings Program (MSSP) with a major focus on fast-tracking Accountable Care Organizations (ACOs) into risk-based contracts. With 477 ACOs now serving over 11.2 million beneficiaries, this overhaul signals a seismic shift in how Medicare accountable care organizations 2026 must operate to thrive in a rapidly evolving healthcare environment.
CMS’s Vision for Value-Based Care in 2026
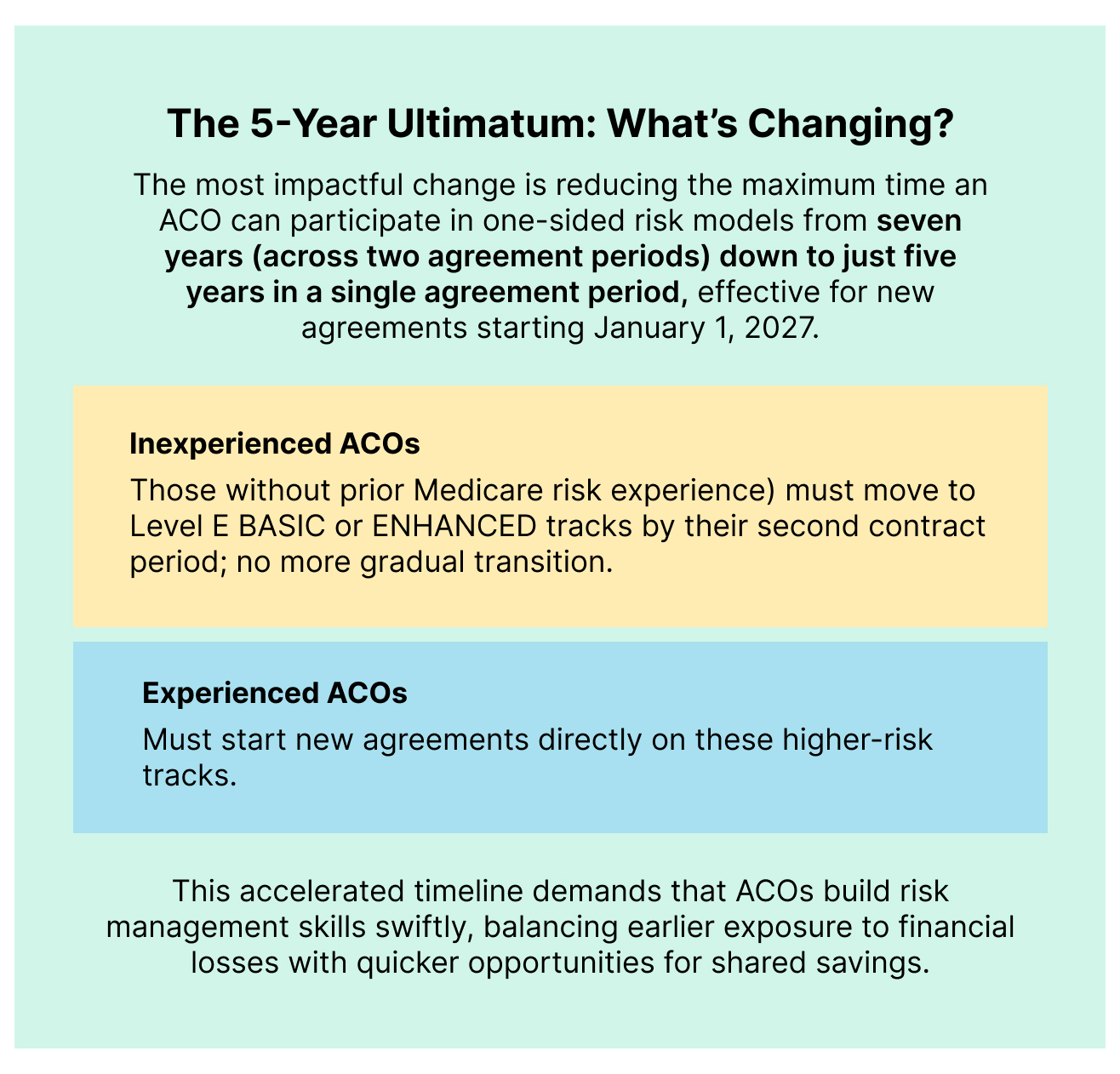
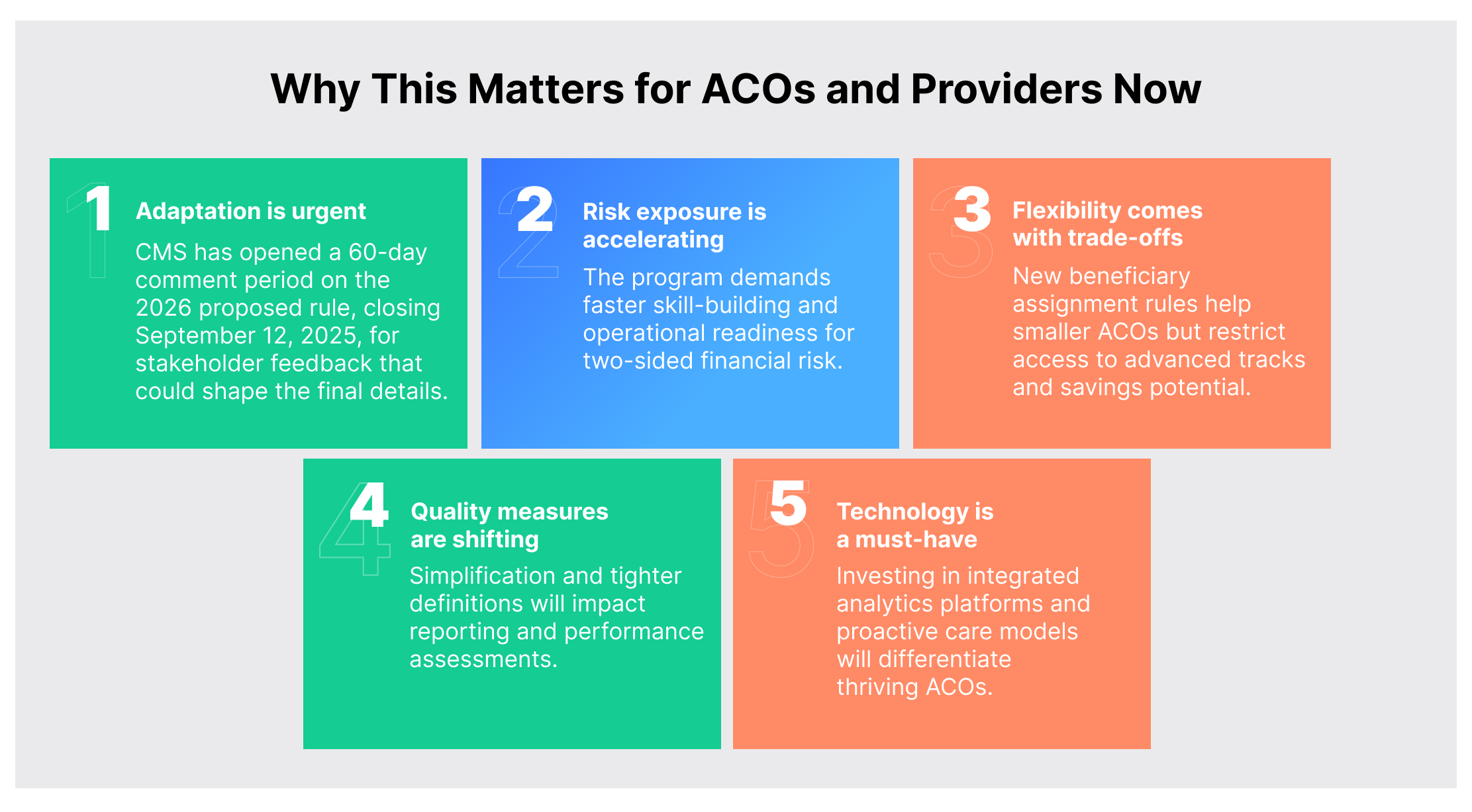
CMS is pushing hard to accelerate the shift from cautious, one-sided risk agreements toward mandatory two-sided risk arrangements. This shift aligns with broader healthcare trends aiming for improved chronic disease management, more efficient resource use, innovation, and greater savings for the Medicare Trust Fund. After years of learning from MSSP’s earlier stages, CMS determined the program is mature enough to require quicker risk adoption from ACOs participating in alternative payment models 2026 CMS has been promoting.
New Flexibility with Limits
In the MSSP 2026 Proposed Rule, CMS is easing beneficiary assignment rules by requiring ACOs to meet the 5,000 beneficiary minimum only in the third benchmark year, rather than every benchmark year. This helps smaller or rural ACOs grow their patient base more flexibly and encourages participation in underserved markets.
However, safeguards apply:
· ACOs that drop below 5,000 beneficiaries in any benchmark year must participate only in the BASIC track.
· They face caps on savings/losses and exclusion from benefits designed for low-revenue organizations.
· These ACOs cannot join the ENHANCED track, limiting advanced participation options.
CMS Quality Measure Updates 2026: The Strategic Impact
The Medicare quality reporting requirements 2026 include:
· As per the MSSP 2026 Proposed Rule, CMS will remove the health equity adjustment from ACO quality scores effective Performance Year 2025, as it overlaps with existing incentives and complicates scoring. This simplification emphasizes core performance data.
· The APP Plus quality measure set will drop the social determinants screening measure (Quality ID 487), signaling a strategic pivot to tighter clinical focus.
· Medicare Clinical Quality Measures eligibility will be tightened to beneficiaries receiving at least one primary care service annually from designated providers. Importantly, primary care now officially includes behavioral health integration and psychiatric collaborative care management, underscoring mental health’s role in value-based care.
· Starting 2026, CMS will expand monitoring to include both standard and alternative quality performance standards, enhancing oversight of ACO performance across multiple frameworks.
ACO risk management strategies 2026: Data, Technology, and Strategy
With a compressed timeline to embrace risk, ACOs must rapidly advance data integration and analytics capabilities. Moving from reactive care to proactive, continuous population health management is no longer optional; it’s critical to survive and thrive.
Strategically, ACOs need frameworks that continuously assess provider network strengths, population features, and historical trends to optimize participation in value-based models and maximize both quality outcomes and financial returns. Agile adjustments based on ongoing performance data are key.
How Persivia Powers ACO Success in the Accelerated Risk-Based Landscape
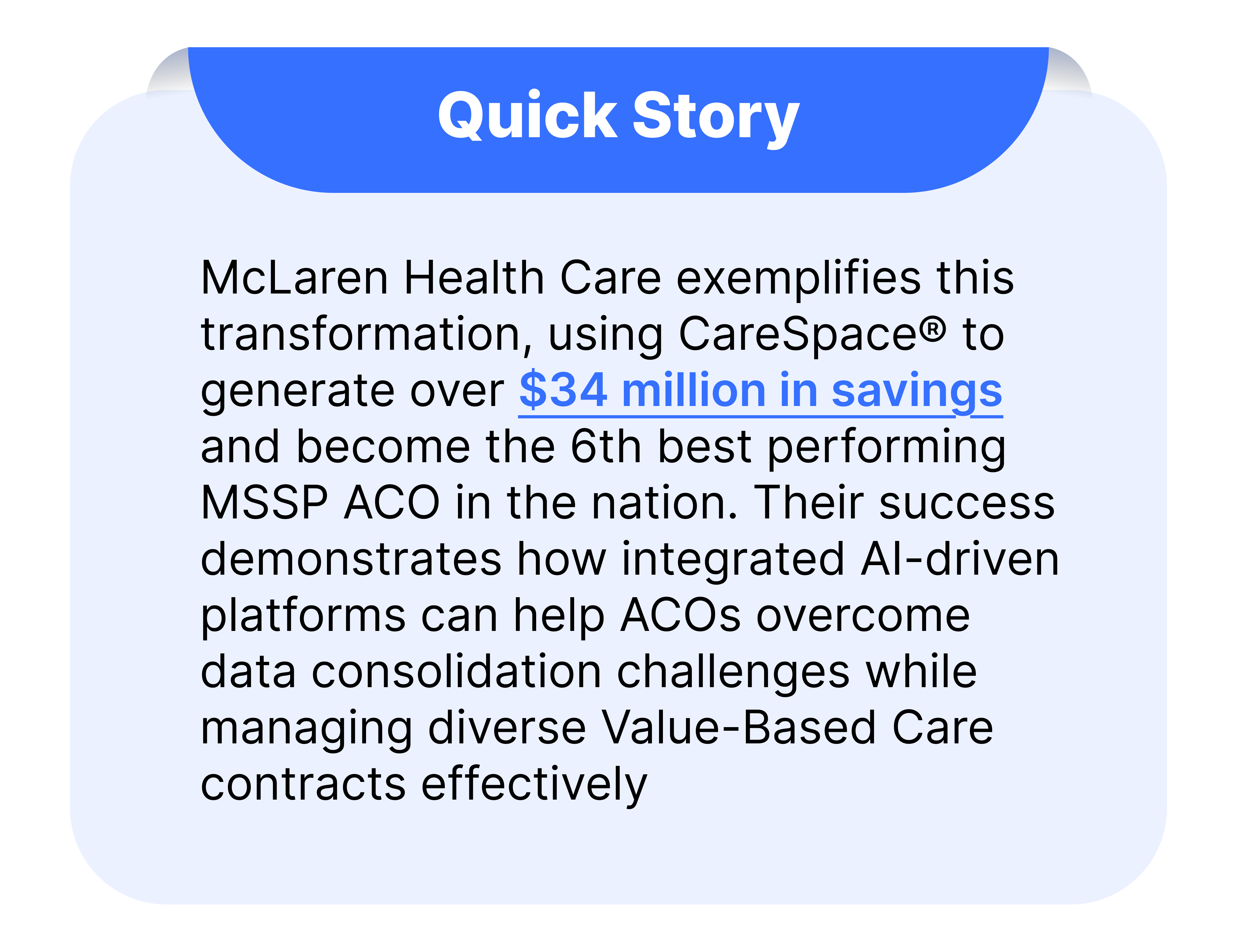
Persivia has been empowering ACOs participating in the MSSP for years, supporting their shift to value-based care by seamlessly integrating clinical and claims data through robust data aggregation and analytics capabilities. CareSpace® is a digital health platform that delivers comprehensive visibility into population health, enabling early identification of high-risk patients and continuous monitoring across critical benchmarks. This powerful platform brings together data from EHRs, clinical systems, and SDoH to create longitudinal patient records, facilitating evidence-based risk management and tailored optimization strategies that drive proactive, rather than reactive, care.
As Medicare rules accelerate ACOs’ migration to risk-based contracts, tightening participation timelines, limiting one-sided risk duration, and enacting more rigorous quality reporting standards, Persivia’s advanced quality management and real-time reporting solutions ensure compliance, efficient CQM submission, and improved reimbursement outcomes.
Conclusion: The New ACO Reality
The voluntary participation era in Medicare’s value-based care programs is ending, and risk-bearing arrangements are becoming mandatory for sustained participation. The five-year countdown to two-sided risk has begun, and organizations that start planning to move to Medicare ACO risk-based contracts now will have significant advantages over those that delay.
Success in this new environment requires early preparation, strategic partnerships, and operational excellence supported by sophisticated technology platforms. The organizations that invest in comprehensive data capabilities, proactive care models, and advanced quality reporting today will be the ones that thrive in tomorrow’s risk-based healthcare landscape.
The message from CMS is unmistakable: adapt quickly or risk being left behind. The question isn’t whether this transformation will happen, but whether your ACO will be ready when it does.
Book a personalized demo to see how Persivia helps your ACO navigate MSSP 2026 rule changes and accelerate risk readiness.
Table of Contents
