LEAD Model vs ACO REACH – ACO REACH wraps up December 31, 2026, and the LEAD Model kicks off January 1, 2027. This new model runs for 10 years, the longest CMS has ever tested, and includes infrastructure payments for rural providers, a simplified approach to specialist partnerships through CARA, and removes some of the barriers that kept smaller ACOs out of ACO REACH.
Introduction
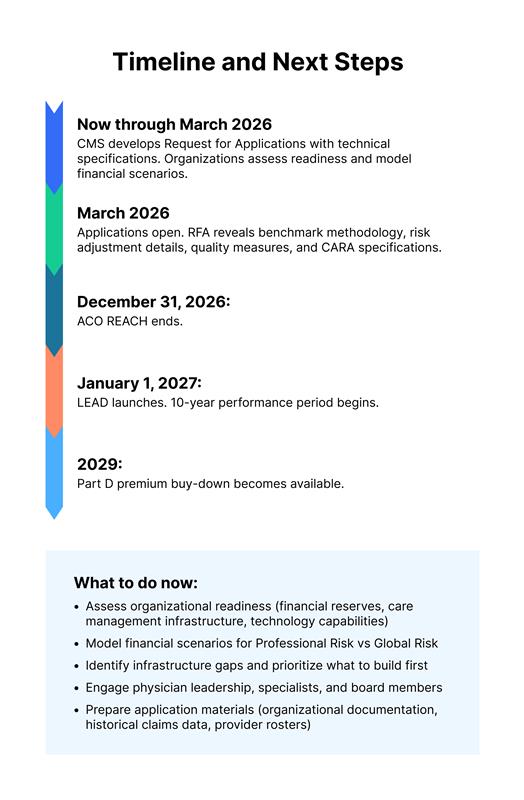
ACO REACH is ending in less than a year. If you’re running one of the 103 participating ACOs, you’re probably already thinking about what comes next. And if you’re a small or rural practice that looked at ACO REACH and decided it wasn’t worth the risk, the replacement model might work for you this time. CMS rolled out the LEAD Model (Long-term Enhanced ACO Design) in December 2025.
This isn’t just a refresh of the old model. CMS spent four years watching ACOs wrestle with unstable benchmarks, administrative headaches, and financial barriers that essentially locked out smaller organizations. (Our whitepaper on the eight barriers to ACO performance breaks down exactly where ACOs get stuck.) They redesigned this from the ground up.
This post walks through what’s changing, what’s staying put, and whether LEAD fixes enough problems to make value-based care viable for organizations that couldn’t participate before.
What’s Changing in the LEAD Model
Here’s what ACO leaders need to understand about how LEAD differs from ACO REACH.
A 10-Year Commitment Instead of a 4-Year Sprint
ACO REACH ran for four years (2023-2026). LEAD runs for 10 years (2027-2036), and here’s the big deal: no rebasing during that entire period.
That decade-long stability means you can actually plan investments in care management infrastructure without worrying that your benchmark will get reset just when you start seeing returns. It’s a fundamentally different planning horizon.
Real Support for Small and Rural Practices
ACO REACH treated everyone the same, which sounds fair until you realize it meant small rural clinics competed on the same terms as large health systems. LEAD changes that approach with specific provisions:
Add-on infrastructure payments that don’t get reconciled later. That means if your savings don’t materialize right away, you’re not paying CMS back for the infrastructure support. Lower beneficiary alignment minimums for new ACO participants, so you don’t need thousands of attributed lives to get started. And full historical spending baselines for first-time ACOs, which matters when you’re trying to establish realistic benchmarks.
Think about a rural health clinic serving 1,500 Medicare beneficiaries. Under ACO REACH, math rarely worked. Under LEAD, they can access infrastructure funding, meet lower alignment thresholds, and plan for a decade instead of trying to break even in year one while still building capabilities.
CARA Makes Specialist Integration Feasible
ACO REACH technically allowed preferred provider arrangements with specialists, but hardly anyone used them. The issue wasn’t permission, it was infrastructure. Building the systems to share data, track episodes, and administer payments was too complex for most ACOs.
LEAD introduces CARA (CMS Administered Risk Arrangements), which handles the operational complexity:
Episode-level data sharing between ACOs and specialists happens through the platform. Standardized contracting templates eliminate the need to negotiate custom agreements. CMS administers payments based on episode performance, taking that burden off ACOs. There’s even a dedicated falls prevention program built in.
Instead of each ACO building custom system to partner with specialists, CMS provides the infrastructure. That’s a meaningful shift.
Risk Adjustment That Accounts for Complexity
One thing ACO REACH got right. The High Needs track. ACOs focused on complex populations including dually eligible beneficiaries, disabled patients, homeless individuals, that were some of the strongest performers in the model. LEAD keeps that track and goes further, integrating high-needs support across all ACOs instead of siloing it.
ACO REACH used standard CMS-HCC risk adjustment, which created a perverse incentive: ACOs serving healthier populations often performed better financially than those caring for sicker patients, even when the latter were delivering better clinical outcomes.
LEAD promises “more accurate risk adjustment integrated across all ACOs” with enhanced benchmarking for complex populations. We’ll see the specific methodologies in the March 2026 Request for Applications, but the intent is clear: serving dually eligible beneficiaries, homebound patients, and other high-complexity populations shouldn’t automatically put you at a financial disadvantage.
Medicaid Integration Begins
ACO REACH focused exclusively on Medicare. LEAD includes a Medicaid integration component, starting with a two-state pilot running from March 2026 through December 2027 to develop ACO-Medicaid partnership frameworks.
For dually eligible beneficiaries—some of the highest-cost, highest-need patients in Medicare—this coordination could mean better outcomes by enabling real care management across both programs instead of the fragmented approach most ACOs are stuck with now.
More Tools for Beneficiary Engagement
LEAD expands what ACOs can offer beneficiaries beyond what ACO REACH allowed:
Part D premium buy-down starting in 2029, which gives ACOs a financial tool to keep high-cost members engaged. Expanded medical nutrition therapy beyond just diabetes and renal disease. Chronic disease prevention rewards that incentivize healthy behaviors. And healthy food products as part of prevention programs, which address social determinants more directly than most current models allow.
These aren’t game changers on their own, but they give ACOs more ways to keep high-risk beneficiaries engaged with primary care instead of showing up in the emergency department when things get bad.
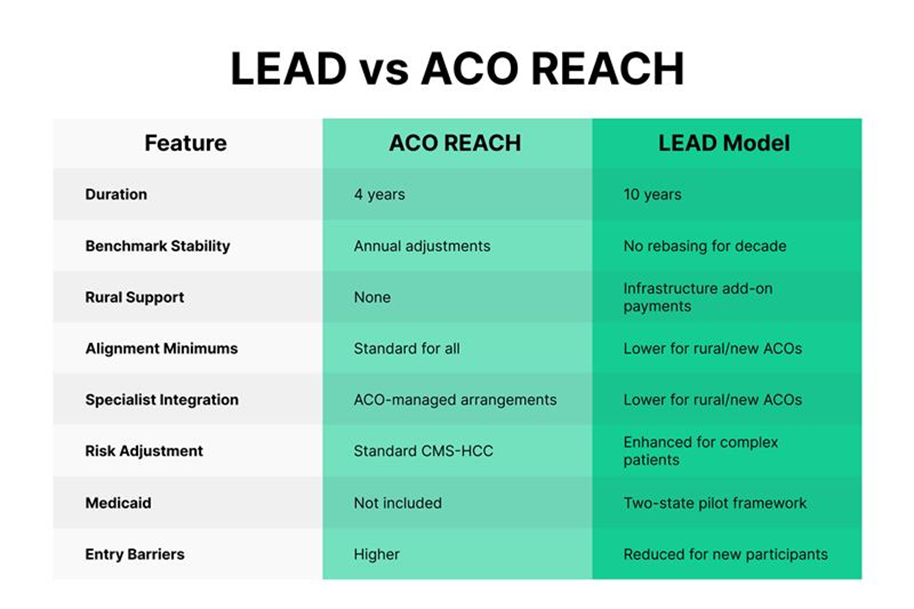
What’s staying the same: Global Risk (100%) and Professional Risk (50%) options, population-based payments, total cost of care accountability, quality performance requirements, and voluntary participation.
Who Should Consider LEAD
Current ACO REACH participants: REACH ends December 31, 2026. LEAD offers the most direct continuation path with 10-year stability and improvements in specialist integration, risk adjustment, and rural support.
Small and independent practices: If an ACO avoided ACO REACH due to financial barriers, LEAD includes infrastructure support and lower alignment minimums designed specifically for this situation.
Rural providers: Add-on payments that aren’t reconciled mean ACOs can build care management capabilities without risking financial losses if savings don’t materialize immediately.
FQHCs and safety-net organizations: Enhanced risk adjustment promises better financial support for serving complex, high-needs populations.
Organizations serving dually eligible patients: Medicaid integration pilot states will have frameworks for coordinated care that doesn’t exist today.
Specialists and specialty groups: CARA creates opportunities to participate in value-based care through ACO partnerships without starting your own ACO.
The Technology Foundation LEAD Success Requires
LEAD’s 10-year timeline rewards organizations that can manage risk, cost, quality, and utilization in real time. Here’s where most ACOs struggle: they’re operating on fragmented systems. Multiple tools that don’t talk to each other. Claims data that arrives months late. Care managers working in one platform while quality reporting happens in another. By the time they identify a problem, the opportunity to intervene has passed.
Managing a decade-long model requires unified infrastructure that consolidates analytics, care management, quality tracking, risk stratification, and clinical workflows into a single foundation. Organizations with integrated platforms can focus on outcomes from day one instead of spending years trying to get their data in order.
CareSpace® consolidates analytics, care management, quality tracking, risk stratification, documentation, and referrals into one platform. When CARA rolls out and ACOs need specialist coordination, their workflows are already built. When CMS publishes the risk adjustment methodology, their data’s organized. When identifying rising-risk patients, predictive analytics run in real time.
Frequently Asked Questions
What happens to ACO REACH participants who don’t join LEAD?
ACO REACH ends December 31, 2026. You can transition to LEAD, join Medicare Shared Savings Program (MSSP), or exit ACO models entirely. Each option has different risk profiles and requirements.
Can we switch between Professional Risk and Global Risk during the 10 years?
CMS hasn’t released specifics yet, but previous models allowed risk track changes at performance year boundaries. Details will be in the March 2026 RFA.
How do we know if we qualify for rural infrastructure add-on payments?
CMS will define eligibility criteria in the March 2026 RFA. Generally, rural designation depends on location-based criteria (Rural Health Clinic status, HRSA rural designations, or county-level classifications).
What’s the minimum patient population needed for LEAD?
LEAD includes lower alignment minimums for new ACO participants and rural providers, but specific numbers haven’t been released. The March 2026 RFA will detail minimum beneficiary alignment requirements.
How does CARA work if we don’t have existing specialist relationships?
CARA is designed to facilitate new relationships, not just formalize existing ones. The platform provides standardized frameworks, data sharing, and payment administration so you can partner with specialists without building custom infrastructure.
Will LEAD use the same quality measures as ACO REACH?
CMS hasn’t released the quality measure set yet. Expect details in the March 2026 RFA, including whether there are different measures for different ACO types.
Conclusion
LEAD makes meaningful changes to address why ACO REACH didn’t work for enough organizations. The 10-year timeline removes benchmark uncertainty. Infrastructure support lower financial barriers for rural practices. CARA simplifies specialist engagement. Enhanced risk adjustment supports organizations serving complex populations.
Current ACO REACH participants get continuity with improvements. Organizations that couldn’t make REACH work get more support. New entrants get the most accessible path CMS has created for value-based care.
Applications open in March 2026 for a January 2027 launch. That evaluation window is short. Organizations considering participation need to assess readiness, model scenarios, identify gaps, and engage stakeholders now. (For a comprehensive breakdown of the LEAD Model structure, see our whitepaper: What is the CMS LEAD Model.)
Table of Contents